Tubular reabsorption is the process of reabsorption of water and substances from the urine contained in the lumen of the tubules into the lymph and blood.
The bulk of the molecules are reabsorbed in the proximal nephron. Here, amino acids, glucose, vitamins, proteins, microelements, a significant amount of Na+, C1-, HCO3- and many other substances are almost completely absorbed.
The loop of Henle, distal tubule, and collecting ducts absorb electrolytes and water.
Aldosterone stimulates Na+ reabsorption and K+ and H+ excretion into the renal tubules in the distal nephron, in the distal tubule and cortical collecting ducts.
Vasopressin promotes water reabsorption from the distal convoluted tubules and collecting ducts.
With the help of passive transport, reabsorption of water, chlorine, and urea is carried out.
Active transport is the transfer of substances against electrochemical and concentration gradients. Moreover, a distinction is made between primary active and secondary active transport. Primary active transport occurs with the expenditure of cell energy. An example is the transfer of Na+ ions using the enzyme Na+/K+-ATPase, which uses the energy of ATP. In secondary active transport, the transfer of a substance is carried out due to the energy of transport of another substance. Glucose and amino acids are reabsorbed by the secondary active transport mechanism.
The value of maximum tubular transport corresponds to the old concept of “renal excretion threshold”. For glucose this value is 10 mmol/l.
Substances whose reabsorption does not depend on their concentration in the blood plasma are called non-threshold. These include substances that are either not reabsorbed at all (inulin, mannitol) or are poorly reabsorbed and excreted in the urine in proportion to their accumulation in the blood (sulfates).
Normally, a small amount of protein enters the filtrate and is reabsorbed. The process of protein reabsorption is carried out using pinocytosis. Upon entering the cell, the protein is hydrolyzed by lysosome enzymes and converted into amino acids. Not all proteins undergo hydrolysis; some of them pass into the blood unchanged. This process is active and requires energy. The appearance of protein in the urine is called proteinuria. Proteinuria can also occur under physiological conditions, for example, after heavy muscular work. Basically, proteinuria occurs in pathology with nephritis, nephropathies, and myeloma.
Urea plays an important role in the mechanisms of urine concentration and is freely filtered in the glomeruli. In the proximal tubule, part of the urea is passively reabsorbed due to the concentration gradient that occurs due to the concentration of urine. The rest of the urea reaches the collecting ducts. In the collecting ducts, under the influence of ADH, water is reabsorbed and the concentration of urea increases. ADH increases the permeability of the wall for urea, and it passes into the medulla of the kidney, creating approximately 50% of the osmotic pressure here. From the interstitium, along a concentration gradient, urea diffuses into the loop of Henle and again enters the distal tubules and collecting ducts. Thus, intrarenal urea circulation occurs. In the case of water diuresis, the absorption of water in the distal nephron stops, and more urea is excreted. Thus, its excretion depends on diuresis.
The reabsorption of weak acids and bases depends on whether they are in ionized or non-ionized form. Weak bases and acids in an ionized state are not reabsorbed and are excreted in the urine. The degree of ionization of bases increases in an acidic environment, so they are excreted at a higher rate in acidic urine; weak acids, on the contrary, are excreted more quickly in alkaline urine. This is important because many drugs are weak bases or weak acids. Therefore, in case of poisoning with acetylsalicylic acid or phenobarbital (weak acids), it is necessary to administer alkaline solutions (NaHCO3) in order to convert these acids into an ionized state, thereby facilitating their rapid elimination from the body. For rapid excretion of weak bases, it is necessary to introduce acidic products into the blood to acidify the urine.
Water is reabsorbed in all parts of the nephron passively due to the transport of osmotically active substances: glucose, amino acids, proteins, sodium ions, potassium, calcium, chlorine. As the reabsorption of osmotically active substances decreases, the reabsorption of water also decreases. The presence of glucose in the final urine leads to increased diuresis (polyuria).
The main ion providing passive absorption of water is sodium. Sodium, as mentioned above, is also necessary for the transport of glucose and amino acids. In addition, it plays an important role in creating an osmotically active environment in the interstitium of the renal medulla, due to which urine is concentrated.
The entry of sodium from primary urine through the apical membrane into the tubular epithelial cell occurs passively along electrochemical and concentration gradients. Sodium is removed from the cell through the basolateral membranes actively using Na+/K+-ATPase. Since the energy of cellular metabolism is spent on sodium transport, its transport is primarily active. Sodium transport into the cell can occur through different mechanisms. One of them is the exchange of Na+ for H+ (countercurrent transport, or antiport). In this case, the sodium ion is transferred inside the cell, and the hydrogen ion is transferred outside. Another way of sodium transfer into the cell is carried out with the participation of amino acids and glucose. This is the so-called cotransport, or simport. Partial sodium reabsorption is associated with potassium secretion.
Cardiac glycosides (strophanthin K, oubain) can inhibit the enzyme Na+/K+-ATPase, which ensures the transfer of sodium from the cell to the blood and the transport of potassium from the blood to the cell.
The work of the so-called rotary-countercurrent multiplying system is of great importance in the mechanisms of reabsorption of water and sodium ions, as well as the concentration of urine. After passing through the proximal segment of the tubule, the isotonic filtrate enters the loop of Henle in a reduced volume. In this area, intensive reabsorption of sodium is not accompanied by reabsorption of water, since the walls of this segment are poorly permeable to water even under the influence of ADH. In this regard, urine dilution occurs in the nephron lumen and sodium concentration in the interstitium occurs. Diluted urine in the distal tubule loses excess fluid, becoming isotonic to the plasma. A reduced volume of isotonic urine enters the collecting system, which runs in the medulla, the high osmotic pressure in the interstitium of which is due to the increased sodium concentration. In the collecting ducts, under the influence of ADH, the reabsorption of water continues in accordance with the concentration gradient. The vasa recta passing through the medulla function as countercurrent exchange vessels, taking sodium along the way to the papillae and releasing it before returning to the cortex. In the depths of the medulla, a high sodium content is maintained in this way, ensuring the resorption of water from the collecting system and the concentration of urine.
As a result of the active absorption of most of the osmotically active components of the filtrate, water is reabsorbed through the walls of the tubules, moving due to diffusion, i.e. passively.
To quantitatively characterize the fate of various substances in the nephron, they are compared with the release of substances that are completely filtered in the glomeruli and are subsequently excreted entirely in secondary urine.
Clearance - the coefficient of purification of blood from various substances - is a somewhat arbitrary concept. Quantitatively, it is characterized by the volume of blood plasma that is completely cleared of a particular substance by the kidneys in 1 minute. Clearance is determined by so-called “non-threshold” substances, i.e. substances that are completely excreted during a single passage through the kidneys. Inulin clearance determines the volume of glomerular filtration and is approximately 120 ml/min. The clearance of para-aminohippuric acid is used to assess the effective renal plasma flow and is equal to 600-650 ml/min.
In the proximal part of the nephron, predominantly metabolites are secreted, in the distal part - K, H, and NH4 ions.
Impaired protein reabsorption
Filtered glucose is almost completely reabsorbed by proximal tubule cells and is usually excreted in urine in small quantities. During reabsorption, glucose binds to the transporter (it is phosphorylated) and is transported through the basal part of the cell into the blood. The role of sodium ions and, accordingly, the Na pump is essential.
With hyperglycemia accompanying diabetes mellitus, the glucose content in the blood exceeds the “renal threshold” level of 8 mmol/l, a lot of glucose is filtered through the glomeruli, and enzyme systems are not able to ensure complete reabsorption. Glucosuria develops. True, in advanced cases of diabetes mellitus, glucosuria may not occur due to kidney damage (angiopathy) and decreased filtration. A hereditary defect in the enzyme systems for glucose reabsorption manifests itself in the form of renal diabetes mellitus, a dominantly inherited disease in which glucosuria develops against the background of normal or even low blood glucose levels. Glucosuria may be a consequence of damage to the tubular epithelium during renal ischemia or poisoning with mercury-containing drugs or Lysol.
Impaired protein reabsorption
The protein is reabsorbed in the proximal tubules by pinocytosis, partially degraded, and then low molecular weight components enter the blood. The mechanisms of protein reabsorption have been little studied. In particular, the essential importance of hemodynamics is known. The appearance of protein in the urine is referred to as proteinuria (albuminuria is more common). Temporary low proteinuria up to 1 g/l can occur in healthy individuals after intense prolonged physical work. Persistent and higher proteinuria is a sign of kidney disease. According to the mechanism of development, it is conventionally divided into glomerular and tubular (glomerular and tubular). With glomerular proteinuria, due to an increase in the permeability of the filtering membrane, protein enters in large quantities into the cavity of the Shumlyansky-Bowman capsule, which exceeds the resorption capabilities of the tubular apparatus. When the glomeruli are damaged, moderate proteinuria develops. True, the degree of proteinuria does not reflect the severity of kidney disease. Tubular proteinuria is associated with impaired protein reabsorption due to damage to the tubular epithelium (amyloidosis, sublimate necronephrosis) or impaired lymphatic drainage. Massive proteinuria is observed in nephrotic syndrome, when both glomeruli and tubules are damaged.
(module direct4)
Transport of electrolytes in the nephron
The cells of the proximal nephron reabsorb most of the components of the ultrafiltrate, but the leading role in this process belongs to the reabsorption of sodium with accompanying anions. It is sodium reabsorption that is the most significant function of the kidneys in terms of volume and energy expenditure. Sodium reabsorption largely determines the total amount of urine excreted, the participation of the kidneys in regulating water in the body, osmotic concentration, ionic composition of the blood and other vital indicators. The kidneys filter 1200 g of sodium per day, and the excretion does not exceed 5-10 g. Reabsorption of sodium in various parts of the nephron has pronounced features. Thus, in the proximal sections, where up to 75% of filtered sodium is reabsorbed, its reabsorption is an active process, but it occurs against a low gradient. Reabsorption of sodium in the distal sections occurs against a high concentration gradient, which causes the release of urine containing almost no sodium ions. It has been established that distal sodium reabsorption is regulated by aldosterone, a hormone of the adrenal cortex. The biochemical mechanisms of active transport of sodium ions remain largely unclear. A certain importance is attached to Mg-dependent ATPase, SDH, and alpha-ketoglutarate dehydrogenase.
Disturbances in the reabsorption of sodium ions can develop when aldosterone production is reduced either due to the action of inhibitors (osmotic diuretics) or when the sensitivity of the renal epithelium to aldosterone is reduced. Under such conditions, along with sodium ions, water is also lost with the possible development of dehydration.
The release of potassium ions accounts for about 10% of what is filtered in the glomeruli, and potassium ions are not only reabsorbed, but also partially secreted in the distal tubules.
Osmotic dilution and concentration of urine
From 120 ml of filtrate, 119 ml are reabsorbed in 1 minute. Up to 85% of this amount is reabsorbed in the proximal tubules following osmotically active substances (Na, glucose, etc.), which is defined as “obligatory reabsorption” of water. About 15% is reabsorbed in the distal sections and collecting ducts - “facultative reabsorption”.
The level of obligatory reabsorption may fall if the reabsorption of sodium or glucose ions is impaired (polyuria in diabetes mellitus, prescription of osmotic diuretics Aldoctan). Facultative reabsorption of water is suppressed when there is a lack of ADH or the absence of a reaction of the renal epithelium to the latter (forms of diabetes insipidus).
The kidneys are capable of excreting urine 4 times more hypertonic and 6 times more hypotonic than blood plasma with fluctuations in relative osmotic concentration of 1002-1035. A decrease in the ability of the kidneys to concentrate urine is expressed in the form of hyposthenuria or isosthenuria.
There is a complete cessation of osmotic concentration. The maximum osmotic concentration is 270-330 mmol/l (relative - 1010-1012).
Daily diuresis in healthy adults is about 70% of exogenously administered water. The minimum volume of urine required to excrete waste is 500 ml. Polyuria - excretion of a daily amount of urine more than 2000 ml, oliguria - 400-500 ml, anuria - up to 200 ml.
In the pathogenesis of urinary excretion disorders, the state of nervous and humoral regulation is important. Emotional factors can change diuresis, and activation of excitation processes in the cerebral cortex leads to polyuria, and inhibition leads to coliguria. Polyuria and oliguria can be obtained by conditioned reflex or by hypnotic suggestion.
Quite often in pathological conditions, reflex pain anuria occurs. Reflex inhibition of urination is possible from various reflexogenic zones. In pathogenesis, the reno-renal reflex is of particular importance, when injury or other damage to one kidney causes temporary anuria of the other, undamaged. At the same time, due to the activation of the sympathoadrenal system, the tone of the renal arterioles increases, which leads to a decrease in glomerular filtration.
Hormonal influences are important - thyroxine increases glomerular filtration and, like glucocorticoids, increases diuresis.
Reabsorption in the kidneys is the reverse absorption by the body of substances of various origins from urine. Such substances can be protein, glucose, water, sodium, organic as well as inorganic components. The process of reabsorption of chemicals and other components involves the renal tubules, as well as epithelial cells. If chemicals are breakdown products and are in excess quantities in the body, they are filtered out by epithelial cells. The absorption process is activated in the proximal tubules.
There are several ways in which the body absorbs nutrients:
- Active - reabsorption of glucose, potassium, sodium ions, magnesium, amino acids. The transport process takes place against a concentration, electrochemical gradient.
- Passive - reabsorption of water, bicarbonate, urea. Transport occurs along an electrochemical, osmotic and concentration gradient.
- Transport by pinocytosis - protein reabsorption.
The rate of filtration, as well as the level of transportation of chemical elements and nutrients, directly depends on the quality of nutrition, the nature of the foods consumed, an active lifestyle, and the presence of chronic diseases.
Kinds
The intake of nutritional components is carried out through different channels. In this regard, reabsorption is divided into 2 types.
Proximal
During the process of proximal reabsorption, proteins, amino acids, fortified components and dextrose are transported from primary urine. In this case, complete absorption of substances is observed. Filtration accounts for only 1/3 of the total volume of nutritional components.
- Water reabsorption is a passive method; its speed and quality depend on the presence of hydrochloride and alkali in the filtration products.
- Bicarbonate is transported using active and passive methods. Its speed depends on the area of the internal organ through which urine is distributed. The passage of urine through the tubules is dynamic. Absorption of nutritional components through the membrane is gradual. With passive transport, urine volume decreases and bicarbonate concentration increases.
- The process of reabsorption of dextrose, as well as amino acids, occurs with the direct participation of epithelial cells located in the brush border of the apical membrane. During this process, simultaneous formation of hydrochloride occurs and a reduced concentration of bicarbonate is observed.
- When glucose is released, it binds to transport cells. If the concentration of glucose is increased, then the transporting cells are under stress, as a result of which the component is not transported into the circulatory system.

During proximal function, maximum protein as well as peptide absorption occurs.
Distal
It affects the final composition of urine, as well as the concentration of organic components. At this stage, maximum absorption of alkali and passive transport of calcium, phosphate, potassium, and chloride ions occur.
Possible problems
If inadequate filtration is observed or dysfunction of the filtering organs manifests itself, then this process can lead to the appearance of various pathologies and physiological disorders:
- Disorders of tubular reabsorption. An increase or decrease in the absorption of ions, water or organic substances from the lumen of the tubules. The causes of dysfunction arise due to reduced activity of transporting components, lack of transporters and macroergs, and injury to the epithelium.
- Disruption of the secretion process of epithelial cells. Injury to the distal tubules, damage to tissues and cells of the medulla or renal cortex. The presence of dysfunction is a provocateur for the development of renal and extrarenal syndromes.
- Renal syndromes - occur as a result of diuresis, disturbances in the rhythm of urination, changes in the color and character of urine. Renal syndromes lead to the development of renal failure, tubulopathy, nephritis.
- Polyuria - diuresis, decreased specific gravity of urine.
- Oliguria - a decrease in the volume of daily urine, an increase in the specific gravity of the liquid.
- Hormonal imbalance - active production of the hormone aldosterone provokes an increase in sodium absorption, resulting in the accumulation of fluid in the body, which leads to edema and a decrease in the availability of potassium.
- Pathologies of the structure of epithelial cells - this process is the main cause of dysfunction in the control of urine concentration.
The exact cause of the pathological condition can be determined using a urine test.

Stories from our readers
“I was able to cure my KIDNEYS with the help of a simple remedy, which I learned about from an article by a UROLOGIST with 24 years of experience, Pushkar D.Yu...”
Laboratory evaluation
In order to determine how proximal reabsorption proceeds, it is necessary to indicate the concentration of glucose in the body, that is, its highest value.
- To determine glucose reabsorption, the patient is injected intravenously with a sugar solution, which significantly increases the percentage of glucose in the blood.
- A urine test is being studied. If the level of the compound is 9.5 - 10 mmol/l, then this is normal.
Other testing is performed to determine the process of distal reabsorption:
- The patient should not drink any liquid for a certain period of time.
- A urine test is taken and the condition of the fluid and its plasma is examined.
- After a certain period of time, the patient is injected with vasopressin.
- After this, you are allowed to drink water.
After studying the results of the body's reaction, it is possible to diagnose diabetes insipidus or nephrogenic diabetes.
The normal functioning of the urinary system contributes to the timely and regular removal of toxic substances and waste products from the body. When the first symptoms of impaired renal function appear, you should immediately consult a specialist. Untimely therapy or its complete absence can lead to serious complications and the development of chronic pathological processes.
Tired of fighting kidney disease?

SWELLING of the face and legs, PAIN in the lower back, CONSTANT weakness and fatigue, painful urination? If you have these symptoms, there is a 95% chance of kidney disease.
If you don't care about your health, then read the opinion of a urologist with 24 years of experience. In his article he talks about RENON DUO capsules.
This is a fast-acting German remedy for kidney restoration, which has been used all over the world for many years. The uniqueness of the drug lies in:
- Eliminates the cause of pain and brings the kidneys to their original state.
- German capsules eliminate pain already during the first course of use, and help to completely cure the disease.
- There are no side effects and no allergic reactions.
6132 0
In CF, more than 100 mg of glucose enters the lumen of the nephron every minute, but it is completely absorbed by the cells of the proximal tubule, so glucose is usually not detected in the urine, and its daily excretion does not exceed 130 mg. Reabsorption of glucose into the blood occurs against a high concentration gradient, since ultimately no glucose remains in the tubular fluid.
The process of glucose transport belongs to the category of secondary active. This is due to the fact that the transfer of glucose from the lumen of the tubule through the brush border membrane occurs using a transporter that requires the presence of a sodium ion. In the brush border membrane, there is no active transport of either glucose or sodium, which is necessary for glucose reabsorption. Cellular energy for this process is created by the operation of the sodium pump, which removes sodium from the cell and is localized in the plasma membranes of the lateral and basal parts of the cell, i.e., facing the intercellular fluid and blood capillaries.
As a result of active transport of sodium from the cell in its cytoplasm, the sodium concentration decreases. This serves as a prerequisite for the passive, gradient entry of sodium into the cell through the brush border membrane. The transporter can transport glucose from the tubular fluid into the cell only when it combines with both glucose and sodium, which allows it to cross the membrane, and from the inside of the cell glucose and sodium are released into the cytoplasm.
Thus, the sodium pump of the basolateral membranes serves as a source of energy. It is the transport of sodium that consumes the energy of TF, which is used for the simultaneous coupled transport of glucose into the cell. Thus, the primary active transport of sodium ensures the secondary active coupled transport of glucose into the cell. This glucose reabsorption system is localized only in the brush border membrane, that is, in that part of the plasma membrane of the cell that faces the lumen of the tubule. There is no such glucose transport mechanism in the basal and lateral plasma membranes. Glucose entering the cell accumulates in the transport fund, where its concentration becomes higher than in the extracellular fluid. The cell membrane in the basal part has low permeability to glucose; To ensure the reabsorption of sugar, its transfer from the cell is determined by special carriers that transport glucose into the extracellular fluid along a concentration gradient and without expending the energy of cellular respiration.
In the clinic, the kidney's ability to reabsorb glucose serves as one of the important indicators of the functional state of proximal tubule cells and the number of effectively working tubules. Features of glucose reabsorption are closely related to the mechanisms of glycosuria. From the above data on the essence of the glucose reabsorption process, it follows that the maximum number of glucose molecules reabsorbed from the tubular fluid into the blood depends on the number of glucose transporters and the rate of their turnover in the membrane. Obviously, all filtered glucose is reabsorbed until the number of carriers and the speed of their movement in the membrane ensure the transfer of all glucose molecules entering the lumen of the tubule.
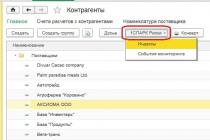
Excretion of glucose in the urine begins only when its concentration in the plasma increases so significantly that the amount of filtered glucose exceeds the reabsorption capacity of the tubules (Fig. 1). The amount of glucose reabsorbed at maximum load of all membrane transporters involved in its transport serves, under standard research conditions, as an important functional indicator of the activity of the proximal tubule. The maximum transport of glucose (TmG) in men is 375±79.7, and in women - 303±55.3 mg/min, calculated per 1.73 m² of body surface.
Rice. 1. The relationship between the concentration of glucose in the blood plasma, its filtration, reabsorption and excretion [Valint R., 1969]. On the y-axis on the left is the amount of filtered, reabsorbed and extracted glucose, on the right is glucose purification; The abscissa axis is the concentration of glucose in the blood plasma.
Studies using glucose infusion and TmG measurements in the clinic provide insight into the balance between CP and reabsorption in the proximal tubule of each nephron. When a hypertonic glucose solution is infused into the blood, hyperglycemia does not cause glucosuria until the limit of its ability to reabsorb glucose is reached in any of the tubules. If in all nephrons there is a correspondence between the volume of filtered fluid (and thereby glucose) and the ability to reabsorb it, then TmG will be achieved simultaneously in all nephrons and with a further increase in the concentration of glucose in the blood, glucosuria occurs.
If the filtration in two nephrons is the same, but the state of the tubules and the ability to reabsorb glucose are different, then TmG will not be achieved simultaneously. The greater the differences between individual nephrons, the more heterogeneous the nephron populations, the less correspondence between the level of glucose CP and its reabsorption, the greater the discrepancy between nephrons in the time of onset of TmG with a gradual increase in plasma glucose concentration. In some nephrons, TmG is achieved at a plasma glucose concentration of 11.1 mmol/l, in others - 22.2 mmol/l. This phenomenon is called splitting of the nephron titration curve with glucose; it depends on the morphological and functional heterogeneity of nephron populations in the kidney.
TmG increases with acromegaly, after administration of thyroxine, and its decrease is characteristic of Addison's disease, serum sensitization, and an increase in the concentration of 1-lysine and 1-alanine in the filtrate. During the course of the disease, the relationship between the volume of CP and tubular reabsorption of glucose may change. In patients with diabetes mellitus, glycosuria may decrease in the dynamics of the disease, despite the constantly high level of glucose in the plasma, which is caused by deposits of protein-mucopolysaccharide complexes in the glomerular capillaries with the formation of iptercapillary glomerulosclerosis in elderly people with long-term diabetes. This causes a decrease in CF in individual nephrons, reduces the load on the tubules with glucose and they have time to reabsorb the filtered glucose, which leads to a decrease in glucosuria.
Clinical Nephrology
edited by EAT. Tareeva
The removal of metabolic products from the body occurs through urine formation, which is based on the reabsorption of previously filtered compounds. It is through reabsorption that blood homeostasis is maintained and final urine is formed with breakdown products of protein substances, ions, toxins and drug components.
Reabsorption is an important process in the kidneys for the reabsorption of blood particles and the formation of final urine with unnecessary and excess substances, which are then eliminated from the human body.What is reabsorption?
To better understand the process, it is necessary to navigate the mechanism of operation of the renal structures and. In the structural and functional unit of the organ, the nephron, three processes continuously occur that maintain the ionic constancy of the blood and ensure the removal of metabolic products from the human body. During filtration, primary urine is formed, which passes from the blood plasma into Bowman's capsule. Next, the reabsorption process itself occurs - the reabsorption of water, protein molecules, glucose, and some organic and inorganic compounds in the kidney tubules into the blood vessels, accompanied by secretion. That is, the second stage of urine formation follows - the transport of substances necessary to maintain homeostasis from primary urine back into the lymph and plasma.
Types of reabsorption in the kidneys
In the nephron, the cells of each region perform different functions due to the different structure of the renal tubules. Based on the anatomical features of the filtration system, two types of reverse absorption are distinguished, which have differences in the types and quantities of transported substances, as well as in the mechanisms of regulation of processes, which are determined by osmotic pressure, the content of certain ions in the urine and antidiuretic hormones.
Proximal suction
In the tubular epithelium, intensive reabsorption of water occurs by a passive method under the influence of alkali and hydrochloride content, thereby reducing the volume of primary urine elements by 1/3. The passage of substances occurs through highly permeable tubular walls. During proximal reabsorption, ions of sodium, chlorine, potassium, bicarbonates, proteins with amino acids, urea products, dextrose and vitamins are transferred. Based on the degree of tubular transport, the classification of urine components is distinguished:
- Threshold. Reabsorption of glucose, proteins, amino acids requires the presence of special renal carrier molecules, connecting with which it becomes possible for the formed complex to pass through the membrane of tubular epithelial cells. If the content of the substance in the urine formed after filtration is greater than the number of necessary molecules, the renal excretion threshold is exceeded and further transport becomes impossible.
- Non-threshold compounds are reabsorbed in a much smaller volume (urea) or are completely unabsorbed, therefore not having their maximum threshold.
Distal reabsorption
The volume of absorbed substances is significantly reduced, but it is this process that determines the composition and concentration of the final urine.
Reabsorption of sodium, calcium, potassium and phosphates occurs actively, while chlorine is characterized by passive transport. The permeability of the membranes of the distal tubules of the nephron is regulated by vasopressin, which directly affects the digestibility of the amount of urea and its entry into the intercellular substance.
What is the mechanism of the process and what does it depend on?
 The mechanism of reabsorption in the kidneys occurs due to the laws of physics, chemistry and energy of the body.
The mechanism of reabsorption in the kidneys occurs due to the laws of physics, chemistry and energy of the body. The speed and quality of reabsorption is influenced by the content of plasma proteins, glucose, some ions and other compounds, the quality of nutrition, lifestyle, the state of the excretory system and the presence of certain diseases. There are several ways of transporting substances through the wall of the renal tubules, on the basis of which the following types of transport are distinguished:
| View | Transferred Substances | Processes at the core |
|---|---|---|
| Active | Glucose, potassium, magnesium | Substances are reabsorbed from the zone of their lower concentration to the zone of high concentration, the body’s energy is expended |
| Passive | Water, urea, bicarbonates | Substances move from a zone of low concentration to a zone of high |
| Pinocytosis | Squirrels | The substance interacts with receptors and is captured by the epithelial membrane in the renal tubules |
What violations can you encounter?
Depending on the etiology and mechanism of the pathological process, the following main groups of causes of reabsorption disorders can be distinguished:
- renal failure, inflammatory and dystrophic processes in the organ, pathologies directly in the tubules;
- nephrotic and nephritic syndromes accompanied by impaired urination;
- pathologies of the endocrine system, and especially disturbances in the synthesis of hormones that affect ion exchange;
- changes in the concentration of certain compounds (glucose, hydrogen) in the urine.