Chronic obstructive pulmonary disease (COPD) is a disease in which there is a partial restriction of airflow in the airways. The changes are irreversible, COPD poses a threat to human life.
Key points:
In severe COPD, the blood gas composition is determined.
If therapy is ineffective, sputum is taken for bacteriological analysis.
Treatment
Chronic obstructive pulmonary disease is an incurable disease. However, adequate therapy can reduce the frequency of exacerbations and significantly prolong the patient's life. For the treatment of COPD, drugs are used that expand the lumen of the bronchi and mucolytic agents that thin phlegm and promote its excretion from the body.
To relieve inflammation, glucocorticoids are prescribed. However, their long-term use is not recommended due to serious side effects.
During the period of exacerbation of the disease, if its infectious nature is proven, antibiotics or antibacterial agents are prescribed, depending on the sensitivity of the microorganism.
Patients with respiratory failure are prescribed oxygen therapy.
Chronic obstructive pulmonary disease (COPD) is a life-threatening disease. The number of deaths per year worldwide reaches 6% of the total number of deaths.
This disease, which occurs with long-term damage to the lungs, is currently considered incurable, therapy can only reduce the frequency and severity of exacerbations, and reduce the level of deaths.
COPD (Chronic Obstructive Pulmonary Disease) is a disease in which airflow is restricted in the airways, which is partially reversible. This obstruction is constantly progressing, decreasing lung function and leading to chronic respiratory failure.
In contact with
Who has COPD
COPD (chronic obstructive pulmonary disease) mainly develops in people with many years of smoking history. The disease is widespread throughout the world, among men and women. The highest mortality is in countries with a low standard of living.
The origin of the disease
With long-term irritation of the lungs with harmful gases and microorganisms, chronic inflammation gradually develops. The result is a narrowing of the bronchi and destruction of the alveoli of the lungs. In the future, all the respiratory tract, tissues and vessels of the lungs are affected, leading to irreversible pathologies that cause a lack of oxygen in the body. COPD (chronic obstructive pulmonary disease) develops slowly, progressing steadily over many years.
If untreated, COPD leads to disability and then death.
The main causes of the disease

- Smoking is the main cause of up to 90% of cases;
- professional factors - work in hazardous industries, inhalation of dust containing silicon and cadmium (miners, construction workers, railway workers, workers of metallurgical, pulp and paper, grain and cotton processing enterprises);
- hereditary factors - rare congenital α1-antitrypsin deficiency.
- Cough Is the earliest and most often underestimated symptom. At first, the cough is periodic, then it becomes daily, in rare cases it appears only at night;
- - appears in the early stages of the disease in the form of a small amount of mucus, usually in the morning. With the development of the disease, the sputum becomes purulent and more and more abundant;
- dyspnea - is found only 10 years after the onset of the development of the disease. At first, it manifests itself only with serious physical exertion. Further, the feeling of lack of air also develops with minor body movements, later severe progressive respiratory failure appears.

The disease is classified according to severity:
Light - with mild impairment of lung function. A minor cough appears. At this stage, the disease is very rarely diagnosed.
Moderate severity - increased obstructive disorders in the lungs. Shortness of breath appears with physical. loads. The disease is diagnosed upon treatment of patients in connection with exacerbations and shortness of breath.
Severe - severe air restriction occurs. Frequent exacerbations begin, shortness of breath increases.
Extremely severe - with severe bronchial obstruction. The state of health greatly deteriorates, exacerbations become threatening, disability develops.
Diagnostic methods

Anamnesis collection - with an analysis of risk factors. In smokers, the smoker's index (IC) is assessed: the number of daily smoked cigarettes is multiplied by the number of years of smoking and divided by 20. IC more than 10 indicates the development of COPD.
Spirometry - to assess lung function. Shows the amount of air during inhalation and exhalation and the speed of entry and exit of air.
Test with a bronchodilator - shows the likelihood of reversibility of the process of narrowing the bronchus.
X-ray examination - establishes the severity of pulmonary changes. The same is done.
Sputum analysis - to determine microbes during an exacerbation and the selection of antibiotics.
Differential diagnosis
X-ray data are also used to differentiate from tuberculosis, as well as sputum analysis and bronchoscopy.
How to treat a disease
General rules
- Smoking must be stopped forever. If you continue to smoke, no treatment for COPD will be effective;
- the use of personal protective equipment for the respiratory system, reducing, if possible, the number of harmful factors in the working area;
- rational, good nutrition;
- reduction to normal body weight;
- regular exercise (breathing exercises, swimming, walking).
Treatment with drugs

Its purpose is to reduce the frequency of exacerbations and the severity of symptoms, to prevent the development of complications. As the disease progresses, the scope of treatment only increases. Essential drugs for COPD treatment:
- Bronchodilators are the main drugs that stimulate the expansion of the bronchi (atrovent, salmeterol, salbutamol, formoterol). Preferably administered by inhalation. Short-acting drugs are used as needed, long-acting drugs are used constantly;
- glucocorticoids in the form of inhalation - used in severe disease, with exacerbations (prednisolone). With severe respiratory failure, attacks are stopped with glucocorticoids in the form of tablets and injections;
- vaccines - Vaccination against influenza can reduce deaths in half. It is carried out once in October - early November;
- mucolytics - thin the mucus and facilitate its excretion (carbocisteine, ambroxol, trypsin, chymotrypsin). Used only in patients with viscous sputum;
- antibiotics - used only for exacerbation of the disease (penicillins, cephalosporins, possibly the use of fluoroquinolones). Pills, injections, inhalations are used;
- antioxidants - able to reduce the frequency and duration of exacerbations, are used in courses of up to six months (N-acetylcysteine).
Surgery
- Bullectomy - removal can reduce shortness of breath and improve lung function;
- reduction of pulmonary volume by surgery - is under study. The operation can improve the physical condition of the patient and reduce the percentage of mortality;
- lung transplant - effectively improves the quality of life, lung function and physical performance of the patient. Application is hampered by the problem of donor selection and the high cost of the operation.
Oxygen therapy

Oxygen therapy is carried out to correct respiratory failure: short-term - with exacerbations, long-term - with the fourth degree of COPD. With a stable course, constant long-term oxygen therapy is prescribed (at least 15 hours daily).
Oxygen therapy is never prescribed to patients who continue to smoke or suffer from alcoholism.
Treatment with folk remedies

Herbal infusions... They are prepared by brewing a spoonful of collection with a glass of boiling water, and each is taken within 2 months:
√ 1 part sage, 2 parts chamomile and mallow each;
√ 1 part linseed, 2 parts each eucalyptus, linden flowers, chamomile;
√ 1 part chamomile, mallow, sweet clover, anise berries, licorice and marshmallow roots, 3 parts flaxseed.
- Infusion of radish. Grate black radish and medium-sized beets, mix and pour over cooled boiling water. Leave on for 3 hours. Drink 50 ml three times a day for a month.
- Nettle. Grind nettle roots into gruel and mix with sugar in a 2: 3 ratio, leave for 6 hours. The syrup removes phlegm, relieves inflammation and relieves cough.
- Milk:
√ With a glass of milk, brew a spoonful of cetraria (Icelandic moss), drink during the day;
√ in a liter of milk, boil 6 chopped onions and a head of garlic for 10 minutes. Drink half a glass after meals. every mother must know!
Coughing spells keep you awake at night? You may have tracheitis. You can learn more about this disease
Secondary
- physical activity, regular and dosed, aimed at the respiratory muscles;
- annual vaccination with influenza and pneumococcal vaccines;
- constant intake of prescribed drugs and regular examinations by a pulmonologist;
- correct use of inhalers.
Forecast
COPD has a conditionally poor prognosis. The disease progresses slowly but steadily, leading to disability. Treatment, even the most active, can only slow down this process, but not eliminate the pathology. In most cases, treatment is lifelong, with ever-increasing doses of drugs.
With continued smoking, the obstruction progresses much faster, significantly reducing life expectancy.
The incurable and deadly COPD simply encourages people to quit smoking forever. And for people at risk, there is only one advice - if you find signs of the disease, immediately contact a pulmonologist. After all, the earlier the disease is detected, the less the likelihood of premature death.
Pathophysiological changes in COPD include the following pathological changes:
- hypersecretion of mucus,
- dysfunction of the cilia,
- bronchial obstruction,
- destruction of the parenchyma and emphysema of the lungs,
- gas exchange disorders,
- pulmonary hypertension,
- pulmonary heart,
- systemic manifestations.
Hypersecretion of mucus
Hypersecretion of mucus is caused by stimulation of secreting glands and goblet cells by leukotrienes, proteinases, and neuropeptides.Cilia dysfunction
The ciliated epithelium undergoes squamous cell metaplasia, which leads to impaired mucociliary clearance (impaired evacuation of sputum from the lungs). These initial manifestations of COPD can persist for many years without progressing.Bronchial obstruction
The following causes of bronchial obstruction are distinguished:- Irreversible:
- Airway remodeling and fibrosis,
- Loss of elastic traction of the lung as a result of destruction of the alveoli,
- Destruction of alveolar support for the lumen of the small airways;
- Reversible:
- Accumulation of inflammatory cells, mucus and plasma exudate in the bronchi,
- Contraction of the smooth muscles of the bronchi,
- Dynamic hyperinflation during exercise.
Pulmonary hyperinflation
Pulmonary hyperinflation (PHI) - an increase in the airiness of the lung tissue, the formation and increase of an "air cushion" in the lungs. Depending on the cause of the occurrence, it is divided into two types:Static PHI: due to incomplete emptying of the alveoli on exhalation due to a decrease in elastic traction of the lungs
Dynamic PHI: due to a decrease in expiratory time under conditions of pronounced restriction of expiratory airflow.From the point of view of pathophysiology, PHI is an adaptive mechanism, as it leads to a decrease in airway resistance, improved air distribution and increased minute ventilation at rest. However, LGI leads to the following adverse consequences:
Weakness of the respiratory muscles. The diaphragm is shortened and flattened, which makes its contraction ineffective.
Restriction of the increase in tidal volume during exercise. In healthy people, during exercise, the minute volume of respiration increases due to an increase in the frequency and depth of breathing. In patients with COPD, pulmonary hyperinflation increases during exercise, since an increase in NPV in COPD leads to a shortening of expiration, and even more air is retained in the alveoli. Increasing the "air cushion" does not significantly increase the depth of breathing.
Hypercapnia during exercise. Due to a decrease in the ratio of OOL to VC due to a decrease in VC due to PHI, an increase in PaCO2 occurs in arterial blood.
Increasing the elastic load on the lungs.
Pulmonary hypertension. Ultimately, PHI leads to pulmonary hypertension.
Emphysema of the lungs
Destruction of the parenchyma leads to a decrease in the elastic traction of the lungs, and therefore is directly related to the limitation of the air flow rate and an increase in air resistance in the lungs. Small bronchi, losing contact with the alveoli, which were previously in a straightened state, collapse and cease to be passable.Gas exchange disorders
Airway obstruction, parenchymal destruction and pulmonary blood flow disorders reduce the lung capacity for gas exchange, which leads first to hypoxemia and then to hypercapnia. The correlation between the values \u200b\u200bof lung function and the level of arterial blood gases is poorly determined, but with FEV1 more than 1 liter, significant changes in the blood gas composition rarely occur. In the initial stages, hypoxemia occurs only with physical exertion, and as the disease progresses, even at rest.Pulmonary hypertension
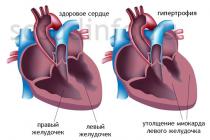
Pulmonary hypertension develops at stage IV - an extremely severe course of COPD, with hypoxemia (PaO2 less than 8 kPa or 60 mm Hg) and often also hypercapnia. This major cardiovascular complication of COPD is associated with a poor prognosis. Usually, in patients with severe COPD, the pressure in the pulmonary artery at rest is moderately elevated, although it can increase with exercise. The complication progresses slowly, even without treatment. The development of pulmonary hypertension is related to vasoconstriction of the lungs and thickening of the vascular wall due to remodeling of the pulmonary arteries, destruction of pulmonary capillaries in emphysema, which further increases the pressure required for blood to pass through the lungs. Vasoconstriction can occur due to hypoxia, which causes contraction of the smooth muscles of the pulmonary arteries, disruption of the mechanisms of endothelium-dependent vasodilation (decrease in NO production), and pathological secretion of vasoconstrictor peptides. Vascular remodeling is one of the main reasons for the development of pulmonary hypertension, in turn, due to the release of growth factors or due to mechanical stress during hypoxic vasoconstriction.Pulmonary heart
Pulmonary hypertension is defined as "right ventricular hypertrophy resulting from diseases affecting the function and / or structure of the lungs, except for those lung disorders that result from diseases primarily affecting the left heart, as in congenital heart diseases." Pulmonary hypertension and reduction of the vascular bed due to emphysema lead to hypertrophy of the right ventricle and its failure only in some patients.Systemic manifestations
In COPD, there is systemic inflammation and skeletal muscle dysfunction. Systemic inflammation is manifested by the presence of systemic oxidative stress, increased concentrations of circulating cytokines, and activation of inflammatory cells. Skeletal muscle dysfunction is manifested by loss of muscle mass and various bioenergetic disorders. These manifestations lead to limitation of the patient's physical capabilities, reduce the level of health, worsening the prognosis of the disease.General characteristics and clinical picture of chronic obstructive pulmonary disease, its causes and development factors. Etiology and pathogenesis of this disease, the principles of diagnosis. Drawing up a treatment regimen and prognosis, prevention of relapse.
Send your good work in the knowledge base is simple. Use the form below
Students, graduate students, young scientists using the knowledge base in their studies and work will be very grateful to you.
Posted on http://www.allbest.ru/
Historyillness
Clinical diagnosis:
Main disease: COPD, emphysematous type, severe course (III stage), exacerbation of moderate severity.
Complications: Emphysema of the lungs. Pneumosclerosis.
Accompanying illnesses: Hypertension stage 3 with arterial hypertension 2 degree, risk 4. Peptic ulcer and12 - tyduodenal ulcer, remission. Dorsopathy of the thoracic spine. Chronic hypertrophic laryngitis.
1. Complaints
At the time of supervision, the patient complains of coughing throughout the day, less often observed at night, with a small amount of mucous sputum, more often in the morning. During and after coughing, shortness of breath occurs.
2. History of the present disease
chronic disease easy relapse
Considers himself ill for several years since 2006, when, against the background of ARVI, a cough appeared throughout the day with discharge of mucopurulent sputum, more often in the morning, progressive shortness of breath. The patient went to the polyclinic at his place of residence, where, after examination, he diagnosed moderate bronchial asthma and prescribed treatment. For this disease, he is constantly taking Seretide, Berotek and Ditek. He felt worsening of his condition since September 2013, when shortness of breath and cough increased, exercise tolerance decreased, associated with an increase in the number of attacks to daily. He underwent inpatient treatment at the place of residence. Despite the treatment, the patient's state of health did not improve, cough with discharge of mucopurulent sputum, increased shortness of breath, given the lack of effect of the therapy, the patient was hospitalized in the therapeutic department for further treatment and examination. On admission, the patient complained of shortness of breath with insignificant physical exertion, intermittent cough with yellow-green sputum. Dyspnea attacks occur more often at night, but also in the morning. The attack is stopped with salbutamol. The patient also complained of headaches, dizziness, sweating, fever up to 37.5 degrees.
3. History life
Grew and developed according to age and gender. 12.09.1954 year of birth (59 years old). Born as the only child in the family. At the time of birth, the mother and father are healthy. Has a specialized secondary education. He served in the army for 2 years.
He is married and has no children. He began working at the age of 18, as a welder, carpenter, fitter. He worked night shifts, arrived in a draft. There is a group 2 disability.
The living conditions are good. Nutrition throughout life: full, regular, observes all the rules of hygiene, leads a passive lifestyle. Diseases transferred in childhood: measles, frequent colds. He does not remember about preventive vaccinations.
Bad habits - smokes since 10 years old, about 10 cigarettes a day. Drinks alcohol. Denies other habits.
Hereditary history - the mother suffers from hypertension, the father died at the age of 56 from stomach cancer.
Botkin's disease, tuberculosis, jaundice, venereal diseases are denied. The presence of allergic reactions to drugs - gentamicin, ampicillin, manifests itself in the form of bronchospasm. Shortness of breath occurs when going out into the cold air, into the cold, on varnishes and paints. Since 2006 he has been taking ditek, berotek, salbutamol.
4. Present state (status praesens)
General inspection
one). The condition is satisfactory. Body temperature 36.8 ° C
2). The patient's position in bed is active.
3). Consciousness is clear.
4). Facial expression is calm.
5). Height - 175 cm.Body weight - 115 kg. The physique is hypersthenic. Posture is straight, gait is fast. Body mass index - 37.5 kg / m2.
6). The skin is pale, mild acrocyanosis (violation of blood oxygenation in the lungs leads to an increase in the content of reduced hemoglobin in the tissues). To the touch, the skin is damp. The skin is elastic. There are no skin rashes. Turgor is reduced. Pink nails, no visible changes. The color of the visible mucous membranes is pale pink, there are no rashes. Tactile, pain, temperature sensitivity is preserved, there is no hyperesthesia.
7). The degree of development of subcutaneous fat is excessive. Subcutaneous fat is painless on palpation. Peripheral edema in the lower third of the lower leg on both sides.
8). Lymph nodes: submandibular, occipital, cervical, axillary, supra-, subclavian, are not palpable.
nine). Musculoskeletal system:
muscles: Muscle development is satisfactory. There is no soreness when feeling. They take part in movement symmetrically.
bones: bones are painless when felt and tapped. On examination, there are no deformations.
joints: normal configuration. Swelling, fluctuation (presence of effusion in the joints) are absent. The temperature of the skin over the joints is normal. The joints are painless to touch and move.
The functions of the joints are preserved, there is no crunch when moving. The volume of active and passive movements in all joints and parts of the spine is normal.
Respiratory system
Inspection. Nose: The shape of the nose is not changed. Free breathing through the nose. Deformation of soft tissues, redness and ulceration at the outer edge of the nostrils, no herpitis rash. The condition of the nasal mucosa is satisfactory.
Larynx: No deformities and swelling in the larynx region. The voice is loud, clear.
Chest: The shape of the chest is emphysematous. An increase in the transverse and special anteroposterior chest size, a deployed epigastric angle (more than 90 degrees), a more horizontal direction of the ribs and an increase in intercostal spaces, in the supraclavicular areas there is a pronounced swelling, a significant increase in the intercostal spaces, a decrease in the elasticity of the chest, a tight fit of the shoulder blades to the chest ... The chest is symmetrical.
Breathing: type of breathing is mixed. Respiratory movements are symmetrical. Respiratory rate 23 per minute. Breathing less rhythmic, lengthening the phase of inhalation and exhalation.
Palpation. On palpation, painful areas were not identified. Decreased elasticity of the chest. Voice jitter symmetrical, bilateral attenuation.
Lung percussion
Comparative percussion: On symmetrical areas of the chest, a percussion box sound is noted.
Topographic percussion:
The upper border of the lungs: right left
standing height of the tops in front 6 cm 6 cm
standing height of the tops behind 8 cm 8 cm
Krenig brim width 9 cm 9 cm
Lower lung border:
along the peri-sternal line 7, the intercostal space is not determined
along the mid-clavicular line 7, the rib is not defined
along the anterior axillary line 8 rib 8 rib
mid axillary line 9 rib 9 rib
on the posterior axillary line 10 rib 10 rib
along the scapular line 11 rib 11 rib
along the paravertebral line spinous process spinous process
11 thoracic vertebra 11 thoracic vertebra
Respiratory excursion of the lower edge of the lung
along the mid-clavicular line along the posterior axillary line
along the scapular line
Auscultation. Weakened vesicular breathing is heard on symmetrical areas of the chest. In the lungs, dry rales of different colors are heard throughout all pulmonary fields. Bronchophonia over symmetrical areas of the chest is weakened on both sides.
The cardiovascular system
Examination and palpation of the heart area. Chest deformity and visible pulsation in the heart area were not detected. On examination, the apical impulse and pulsation in the epigastric region are not detected. The apical impulse is palpated in the 5th intercostal space on the left 2 cm medially from lin. medioclavicularis, localized, not spilled, not strengthened. The impulse of the right ventricle and pulsation at the base of the heart are not detected by palpation.
Percussion of the heart. Borders of relative cardiac dullness:
Right - in the 4th intercostal space 1.5 cm outward from the right edge of the sternum;
Upper - at the level of the 3rd rib along l. parasternalis sinistrae;
Left - in the 5th intercostal space 1.5 cm medially from the midclavicular line.
The boundaries of absolute cardiac dullness:
Right - on the left edge of the sternum in the 4th intercostal space;
Upper - at the level of the 4th rib along l. parasternalis sinistrae;
Left - 2 cm inward from l. medioclavicularis in the 5th intercostal space.
Heart diameter: 12 cm (at a rate of 12 - 12.5 cm).
Vascular bundle width: about 5 cm (does not go beyond the sternum in the 1st and 2nd intercostal spaces).
There are 2 basic heart sounds. No splitting and bifurcation of the II tone. Bifurcation of the I tone is absent. There is no canter and mitral valve opening click. Heart rate 70 / min, rhythmic, preserved, tones are weakened in the main places of listening. No pathological murmurs were found.
Research of blood vessels. Pulsations in the area of \u200b\u200bthe sternum handle, "carotid dance", no tortuosity of the arteries. There is no varicose veins of the lower extremities. The coloration of the skin of the extremities is normal. There are no varicose veins. There are no trophic ulcers. The arch and abdominal aorta are not palpable. Arterial pulse on the radial arteries: the same on the radial arteries of both arms, rhythmic, normal frequency - 70 beats per minute, good filling, normal tension, magnitude, speed and shape. There is no pulse deficit. Examination and palpation of arteries in other areas without pathology. The condition of the vascular wall is satisfactory.
The skin temperature of the extremities is normal, the same. The blood pressure on the right brachial artery corresponds to the blood pressure on the left brachial artery and is equal to 110/80.
Digestive system
Examination of the oral cavity. The red border of the lips is of the usual color, there are no rashes. The bite is correct. The gums don't bleed; loosening, ulcers, rashes are absent. Tongue of regular shape, normal size, normal color, without plaque, ulcers and tumors, located in the center. The mucosa is pale pink, shiny, no ulceration. The tonsils are not enlarged. Palatine arch unchanged. There are no hemorrhages and ulcers on the oral mucosa.
Examination of the abdomen. The shape is correct, there is a general increase. Both halves of the abdomen are symmetrical. There are no areas of pigmentation, rash, scratching, hemorrhage. There are no venous collaterals. There are no hernias and discrepancies in the rectus abdominis muscles. The navel is retracted.
Superficial palpation of the abdomen. The abdominal wall is soft, not tense, painless. Hernial protrusions are not noted.
Deep palpation. Cecum located in the middle third of the distance from the navel to the iliac crest; diameter about 3 cm; elastic; the wall is smooth, even, sufficient mobility (2 cm); painless; rumbling is not detected.
Sigmoid colon located correctly; diameter about 2 cm; elastic; the wall is smooth, even, sufficient mobility (3 cm); painless; rumbling is not detected.
Transverse colon, its ascending and descending divisions located correctly; diameter about 2 cm; elastic; the wall is smooth, even, sufficient mobility (2 cm); painless; rumbling is not detected.
Superficial tumors are absent.
Percussion. Percussion sounds in various departments are normal. There are no tumors. There is no free and encapsulated liquid.
Auscultation. Intestinal peristalsis, peritoneal friction noise are not heard.
Liver examination. Visually, the liver and gallbladder are not enlarged, liver pulsation is not detected. Palpation: the edge of the liver is elastic, smooth, sharp, the surface is smooth, no pain. On a deep breath, 1 cm comes out from under the edge of the costal arch along the mid-clavicular line. Percussion upper border of relative dullness along the right peri-sternal line - 6 rib, along the right midclavicular line - 6 rib; along the anterior axillary line - 6 intercostal space. The lower border is at the border of the upper and middle third of the distance from the xiphoid process to the navel. The left border along the edge of the left costal arch does not go beyond the left parasternal line. Dimensions according to Kurlov: 10 * 8 * 9 cm.
Examination of the gallbladder. Not palpable.
Examination of the spleen. There is no visible enlargement of the spleen. Not palpable. Percussion determined:
the upper border is at the level of 9 ribs along the left mid-axillary line;
the lower border is at the level of 11 ribs;
posterior-superior pole - along the line from the spine to the upper border;
antero-lower pole - along the line from the navel to the middle of the distance between the upper and lower boundaries.
Spleen length 11.5 cm; diameter 7 cm.
Examination of the intestinal area revealed no pathological changes.
urinary system
Examination of the bladder. The bladder when viewed without pathology.
Palpation.Palpable painless. There are no pains along the ureters. There are no indications for a special examination of the genitals and rectum.
Examination of the kidneys. Examination of the lumbar region revealed no edema or swelling.
Palpation. With deep palpation standing and lying, the kidneys are not palpable. There is no muscle tension and soreness. Pasternatsky's symptom is negative.
Hematopoietic system
Skin color is pale pink, mucous membranes are pink. No hemorrhages. There is no soreness when tapping on the sternum and tubular bones. The condition of the lymphatic apparatus and spleen is normal. There are no hemic and anemic murmurs in the heart and blood vessels.
Endocrine system
The appearance of the patient according to age. The growth and size of individual parts of the body are normal. Pigmentation of skin and mucous membranes without pathology. Male pattern hair growth. The face is oval, pale pink in color. Subcutaneous tissue is moderately expressed. No striae were found. No edema. Examination revealed no pathologies of the thyroid gland. There is no tremor of the hands, eyelids and tongue. Symptoms of Moebius, Graefe, Shtelvag are negative. On palpation, the thyroid gland is not enlarged, painless. Examination, palpation of the pancreas without pathology. Increased thirst, appetite, no girdle pain. Adrenal glands without pathology. Signs of Addison's disease, weight loss, "bronze" staining of the skin, no general spotty staining, no lowering of blood pressure. There are no signs and symptoms of Itsenko-Cushing's disease.
Nervous system
Consciousness is unchanged. Intelligence, attention, speech are not impaired. There is no soreness of the nerve trunks on palpation. The sensitivity is preserved. Coordination is not broken. There are no paralysis and paresis. Reflexes are unchanged. The reaction of the pupils to light is friendly. There are no meningeal symptoms. Vasomotor disorders, dermographism are absent. Sweating, salivation is normal. Trophic disorders are not observed.
Mental status
The patient's psyche is not disturbed. The mood is good, the behavior is adequate, there is no depression. The memory condition is satisfactory. The character of the patient is calm, the energy is slightly reduced, the mind is preserved, has a wide range of interests, the attitude towards family and other people is good. There are no traumas and conflicts of a psycho-emotional order. Concussions, concussions are absent. Sleep is normal. Changes in the character, well-being and mood of the patient due to the disease are not observed.
5. Isolation of disease syndromes according to clinical examination data
According to the history and objective research, the following syndromes can be distinguished:
Broncho-obstructive syndrome
Bronchitis syndrome
Broncho-obstructive syndrome:
Subjectively: with minor physical exertion, constant dyspnea of \u200b\u200ba mixed nature (expiratory component) occurs, which increases during walking and at night. In addition, an intermittent productive cough that brings relief, with a small amount of hard-to-separate gray, odorless sputum.
Objectively: over the anterior parts of the lungs - rigid vesicular breathing. Above the anterior surface of the lungs (especially on the right), high dry and low wheezing (better - with forced exhalation).
The main pathogenetic factor in the development of bronchial obstruction is a respiratory infection. With an outbreak of bronchial infection, a large number of neutrophilic polynuclear cells accumulate in the lumen of the bronchi. Leukocyte elastase is released into the lumen and peribronchial tissue, as a result of which the elastic elements of the bronchial wall and peribronchial lung tissue are destroyed. In the course of further regenerative processes, their fibrotic changes are observed. The contributing factors here are frequent respiratory infectious diseases in the last 2-3 years, as well as a long smoking history. Thus, "untreated" air enters the respiratory tract, which contributes to hypothermia and drying of the bronchial mucosa. This leads to compensatory mucus hypersecretion and impaired mucocellular clearance. Over time, hyperplasia of the mucous glands of the bronchi develops. As a result of the development of an inflammatory reaction in the wall of the bronchi and the release of inflammatory mediators, the permeability of blood vessels increases, and edema of the bronchial mucosa develops.
A decrease in the lumen of the bronchi ultimately leads to a significant increase in the load on the respiratory system to maintain the necessary ventilation of the alveoli at the proper level. With a decrease in the partial pressure of oxygen in the blood, reflex stimulation of the respiratory center occurs, which leads to an increase in the respiratory rate. And in the presence of obstructive changes in the bronchi, the patient has expiratory dyspnea. The narrowing of the lumen of the bronchi and a change in the relief of their mucous membrane explains the audible rigid vesicular breathing. If there is a very viscous secretion in the lumen of the bronchi, which is firmly held against the walls, dry wheezing is heard.
The onset of cough in a patient is explained by irritation of the reflexogenic zones of the cough center in the larynx, trachea, bronchi with inhaled particles. Impulses from these receptors are transmitted along the n fibers. vagus to the expiratory neurons of the respiratory center, where a certain sequence of coughing phases is formed.
The occurrence of asthma attacks can be explained by bronchospasm as a result of a reflex increase in the tone of the muscles of the bronchi under the influence of various factors (cough, foreign particles, irritating gases), which act directly or through n. vagus (in chronic inflammation, there is a decrease in the sensitivity threshold of these receptors, which determines the hyperactivity of the bronchi in response to minor irritation).
In this patient, shortness of breath appears with minor physical exertion, during and after coughing.
Bronchitis Syndrome: complex subjective-objective-paraclinical syndrome.
Subjectively: periodic productive cough with a small amount of hard-to-separate gray, odorless sputum. The cough brings relief.
Objectively: over the anterior parts of the lungs - rigid vesicular breathing. Above the anterior surface of the lungs (especially on the right), high dry and low wheezing (better - with forced exhalation).
Inflammation of the bronchi in this clinical case, by its etiology, can be bacterial or viral. In any case, humoral or cellular hypersensitivity of the body is possible.
In the case of humoral hypersensitivity, the blood contains antibodies (AT) to the corresponding bacterial (or viral) antigens (AH), and the resulting immune complexes will trigger a cascade of reactions that cause the development of edema of the bronchial mucosa and hypersecretion of the bronchial glands. In the case of cellular hypersensitivity, the connective tissue of the lungs and bronchi will contain cells sensitized to specific AH, the contact of which with AH will also lead to the release of mediators and the development of immune inflammation. If the body is unable to cope with the infection, then persistent hypertension causes a chronic local HNT reaction.
The mechanisms of development of hard vesicular breathing and dry wheezing are given in the description of broncho-obstructive syndrome.
This patient has a frequent cough, less often at night, with a small amount of mucous sputum, more often in the morning. During and after coughing, shortness of breath occurs.
6. Preliminary diagnosis and its rationale
Main disease: COPD, emphysematous type, severe course (stage III), exacerbation of moderate severity .
Complications: Emphysema of the lungs. Pneumosclerosis.
Concomitant diseases: Hypertension stage 3 with arterial hypertension, grade 2, risk 4. Peptic ulcer and 12 duodenal ulcer, remission. Dorsopathy of the thoracic spine. Chronic hypertrophic laryngitis.
Based:
Complaints of coughing throughout the day, less often at night, with a small amount of mucous sputum, more often in the morning. During and after coughing, shortness of breath occurs.
Anamnesis morbi - Considers himself ill for several years since 2006, when, against the background of acute respiratory viral infections, a cough appeared throughout the day with discharge of mucopurulent sputum, more often in the morning, progressive shortness of breath. The patient went to the polyclinic at the place of residence, where, after examination, he diagnosed moderate bronchial asthma and prescribed treatment. He felt worsening of his condition since September 2013, when shortness of breath and cough increased, exercise tolerance decreased, associated with an increase in the number of attacks to daily. He underwent inpatient treatment at the place of residence. Despite the treatment, the patient's state of health did not improve, cough with discharge of mucopurulent sputum, increased shortness of breath, given the lack of effect of the therapy, the patient was hospitalized in the therapeutic department for further treatment and examination. Thus, for several years the patient did not seek medical help, the disease progressed slowly.
Physical examination data - decreased elasticity of the chest. Voice jitter symmetrical, bilateral attenuation. With percussion on symmetrical areas of the chest, a boxed sound is noted. On auscultation, weakened vesicular breathing is heard in symmetrical areas of the chest. In the lungs, dry rales of different colors are heard throughout all pulmonary fields. Bronchophonia over symmetrical areas of the chest is weakened on both sides.
A moderate course is set on the basis of frequent exacerbations of the disease and on the basis of complaints.
A moderate exacerbation is based on the severity of shortness of breath with little physical exertion, yellow-green sputum. Increase in DN - participation in breathing of auxiliary muscles, paradoxical movement of the chest, the appearance and aggravation of central cyanosis, changes in the gas composition of the blood.
7. Plan of additional examination of the patient
I. Laboratory research methods
1) Complete blood count
2) Biochemical blood test (urea, bilirubin, cholesterol, ALT, AST, creatinine, glucose)
3) General urine analysis
4) Blood on RW, HIV
II. Instrumental research methods
1 ) Chest X-ray.
2 ) ECG
8. Additional research results
X-ray. There is an increase and deformation of the pulmonary pattern in the lower right section, which does not exclude infiltration.
Conclusion: Pneumonia in the lower part of the right lung is not excluded.
ECG. Sinus rhythm. Heart rate 60 beats per minute. Incomplete blockade of the right bundle branch block.
General blood analysis.
Hemoglobin 139 g / l
Erythrocytes 4.39x10№І / l
Color Index 0.95
ESR 9 mm / h
Platelets 195x10 / l
Leukocytes 8.1x10 / l
Reticulocytes 5.5%
Conclusion: In the general analysis of blood, pathological changes are not observed.
Biochemical blood test.
Urea 9.21 mmol / l
Bilirubin 7.1 mmol / L
Cholesterol 4.72 mmol / L
ALT 0.18 μmol / L
AST 0.24 μmol / L
Creatinine 98 mmol / L
Glucose 4.0 mmol / L
Conclusion: Biochemical analysis is normal.
General urine analysis.
Quantity: 10 ml
Color: straw yellow
Transparency: full
Reaction: acidic
Protein: negative
Leukocytes: 2-3 cells. in sight
Erythrocytes: fresh. 0-1, modified 10-12
Epithelial cells: 0-1 cells in sight
9. Final justification for sinptomov
Taking into account the laboratory tests carried out, the presence of syndromes can be confirmed. An infiltrative syndrome was also identified, leading to bronchitic syndrome, which in turn leads to bronchial obstruction.
10. Differential diagnosis
In the early stages of COPD, a distinction should be made between COP and AD, because at this time, fundamentally different approaches to the treatment of each of these diseases are required. Differential diagnosis of BA and COB is the most difficult. Clinical examination reveals paroxysmal symptoms in BA, often in combination with extrapulmonary signs of allergy (rhinitis, conjunctivitis, skin manifestations, food allergy). Patients with COB are characterized by constant, little-changing symptoms. An important element of differential diagnosis is a decrease in FEV 1 by 50 ml or more per year in patients with COB, which is not observed in BA. COB is characterized by low daily variability of peak flowmetry parameters (< 15%). При БА разность между утренними и вечерними показателями пикфлоуметрии увеличивается и превышает 20%. При БА чаще наблюдается бронхиальная гиперреактивность. Из лабораторных признаков при БА чаще встречается увеличение содержания IgE.
When an irreversible component of bronchial obstruction appears in BA patients, the differential diagnosis between these diseases loses its meaning, because we can state the addition of the second disease - COP and the approach of the final phase of the disease - COPD.
The main differential diagnostic criteria for COPD and BA.
|
Signs |
||||
|
1. Allergy |
Not typical |
Is characteristic |
||
|
Constant, varying intensity |
Paroxysmal |
|||
|
Constant, without sharp fluctuations in severity |
Expiratory dyspnea attacks |
|||
|
4. Daily changes in FEV1 |
Less than 10% of due |
More than 15% of the due |
||
|
5. Bronchial obstruction |
Reversibility is uncommon, progressive deterioration in lung function |
Reversibility is characteristic, there is no progressive deterioration in lung function |
||
|
6. Eosinophilia of blood and sputum |
Maybe, but not related to the underlying pathology |
Is characteristic |
Let us turn to the formulations that define the essence of these diseases.
AD is a chronic inflammation of the airways with the predominant participation of mast cells, eosinophils and T-lymphocytes, manifested by repeated attacks of wheezing, shortness of breath, chest compression and coughing, which occur mainly at night or in the early morning. These symptoms are usually associated with widespread but variable bronchial obstruction that is reversible (at least partially) spontaneously or as a result of treatment.
COPD is an ecologically mediated chronic inflammatory disease of the respiratory system with a predominant lesion of the peripheral respiratory tract and pulmonary parenchyma with the development of emphysema, manifested by partially reversible bronchial obstruction and characterized by the progression and increasing phenomena of chronic respiratory failure resulting from the pathogenic inhalation of particles or gases.
Common in these diseases is the underlying chronic inflammatory process, which determines the clinical picture of the disease, as well as the methods of diagnosis and treatment. And if in BA the inflammatory process is allergic and is localized mainly in the airways, in COPD a completely different picture is observed.
First of all, the nature of chronic inflammation in COPD is not yet fully understood. It is clear that this is not an allergic inflammation. At the same time, it is impossible to refer it to the category of ordinary chronic inflammatory processes due to its steady progression and environmental mediation.
Distinguishes between COPD and the localization of inflammation. As in AD, inflammation in COPD is localized mainly in the peripheral airways, but unlike AD, it is not limited to this, but spreads to the interstitial tissue and lung parenchyma, leading to the destruction of the alveolar walls and the development of pulmonary emphysema. It is this mechanism that is the main one in the formation of an irreversible component of bronchial obstruction. Therefore, the disease is called "chronic obstructive pulmonary disease", which involves the defeat of all components of the lungs, and not just the airways.
The next important distinguishing feature of COPD is the progressive nature of the course of the disease, which is not typical for classical AD.
Finally, the clinical manifestations. BA is characterized by undulation and reversibility of respiratory symptoms. In COPD, there is a slow but steady increase in shortness of breath, poorly controlled by conventional bronchodilators.
Differential diagnosis of BA and COPD is based on the integration of basic clinic data, results of functional and laboratory tests. There is currently no laboratory marker that reliably differentiates the two diseases. The main emphasis in differential diagnosis is placed on the establishment of the main signs that determine the essence of the disease: in AD, this is the undulation and reversibility of symptoms, and in COPD, it is a steady progression and lack of reversibility.
BA patients are characterized by a classic list of risk factors - allergens that cause the development of the disease. These are household allergens, plant pollen, some production factors, etc. The list of possible causal factors is long and is described in special BA guidelines. As for COPD, smoking is the main risk factor (up to 90%). In recent years, data have appeared on the effect of combustion products of certain types of household fuel, industrial pollution and some production factors (silicon, cadmium).
Most BA patients have a hereditary predisposition, which is not observed in COPD patients. AD can begin in any period of life, and COPD is a disease of the second half of life, and very serious arguments are needed for the diagnosis of COPD at a young age. This is due in part to the cumulative effect of the risk factor over many years.
The most important component of diagnostics is the analysis of clinical manifestations. Here quite definite and fundamental differences come to light.
AD is characterized by a wave-like symptomatology, the brightness of clinical manifestations and their reversibility (spontaneously or under the influence of therapy). The severity of a BA patient's condition is not determined by the length of the illness and may be maximum at the onset of the disease, and then, with adequate therapy, the main symptoms of the disease may disappear completely. With COPD, the disease creeps up gradually, provided the risk factor is long-term. The first symptoms are noticed by the patient usually already in the II stage of the disease.
Certain differences in the social status of an average BA and COPD patient should be emphasized. If a BA patient can belong to any stratum of the population, then COPD most often develops in patients with a low socioeconomic level. This largely determines the reaction of patients to early signs of the disease. Asthmatics are impressionable people, and every minimal sign of the disease, whether it be a "tickling" behind the breastbone, a night coughing fit or an extended attack of suffocation, the patient will certainly not ignore and seek medical help. A patient with COPD, an early sign of the disease - cough in the morning - usually refers to the natural state of a smoking person and does not take any measures, but thinks about his state of health only when shortness of breath develops (this usually happens 8-10 years after the first sign of the disease - coughing) ... Thus, there are prerequisites for the late diagnosis of COPD.
Different principles are also used in the classifications of AD and COPD. In BA, the classification by severity is based on the severity of clinical symptoms, and in COPD, the functional parameter is the basis - the degree of reduction and its relation to FVC. Thus, in BA, functional signs of impaired bronchial patency are factors that complement the diagnosis, and in COPD, they are fundamental for determining the severity (stage) of the disease, which suggests the secondary nature of clinical manifestations with the main role of FVD indicators.
Despite the outward similarity of the clinical manifestations of AD and COPD, there are differences in almost all the main signs, which make it possible to distinguish between these two nosological forms even at the stage of a simple physical examination.
Changes in FVD also highlight the main difference between these diseases - the waveform of symptoms, which is characteristic of AD and is absent in COPD. At the same time, functional changes in COPD are progressive and disabling.
The least distinct differences are observed in the analysis of laboratory parameters of patients with BA and COPD. Eosinophilia and an increase in serum IgE levels, previously considered reliable signs of AD, can also be observed in COPD, which can lead to diagnostic errors.
Thus, the differential diagnosis between BA and COPD should be carried out by summarizing the data of clinical, functional and laboratory studies. A special (and very significant) population is made up of patients who have BA and COPD. In such cases, the meaning of differential diagnosis is lost, and both diseases are diagnosed. In these patients, in fact, there is a summation of the signs of both diseases. Thus, at present, quite simple and reliable criteria for the differential diagnosis of BA and COPD have been developed, which allows avoiding a large number of standard errors.
COPD and other diseases
At certain stages of the development of COPD, especially with a single (first) meeting with a patient, it may be necessary to differentiate COPD from a number of diseases with similar (externally) symptoms.
COPD and pulmonary tuberculosis
A special place is occupied by the differential diagnosis of pulmonary tuberculosis and COPD. Tuberculosis
Joining tuberculosis of the lungs of the defeat of the bronchial tree and bronchial obstruction significantly aggravates the course of the disease. Broncho-obstructive syndrome (BOS) occurs in all forms of pulmonary tuberculosis, the frequency of its detection depends on the duration of the course of a specific process and on the severity of residual changes in the lungs. With focal tuberculosis, bronchial obstruction occurs in 52.7%, with infiltrative tuberculosis - in 56.6%, with fibrous-cavernous - in 76.9%, with disseminated - in 88.2%. The prevalence of biofeedback among persons with post-tuberculosis changes in the lungs ranges from 59.5 to 83.9% - 2-3 times higher than among the rest of the population. BFB is one of the main causes of temporary disability, disability and premature death of these patients.
There are 3 forms of combination of biofeedback with pulmonary tuberculosis:
1. Paratuberculous (preceding pulmonary tuberculosis) due to chronic obstructive bronchitis (COP) or chronic obstructive pulmonary disease (COPD).
2. Metatuberculosis biofeedback, which occurs during long-term active pulmonary tuberculosis.
3. Post-tuberculous biofeedback, which develops after the cure of active tuberculosis against the background of residual post-tuberculosis changes in the lungs.
Thus, in patients with pulmonary tuberculosis, at least the following causes of bronchial obstruction are possible: manifestation of COPD, manifestation of COB, manifestation of tuberculous bronchitis, secondary bronchial obstruction without significant morphological changes in the bronchi. There are no precise epidemiological data on the combination of COPD with pulmonary tuberculosis due to terminological uncertainty that has existed in recent years. Nevertheless, the presence of obvious signs of pulmonary tuberculosis (intoxication, X-ray data, positive tuberculin tests, isolation of mycobacteria) in the presence of biofeedback requires first of all to exclude a specific (tuberculous) damage to the airways. This is easy to do when conducting a bronchological examination.
To establish whether BFB belongs to COPD in patients with pulmonary tuberculosis, it is necessary to establish the presence of the main criteria for COPD in a patient:
chronic inflammation caused by environmental factors (smoking, irritating particles and gases);
damage to the airways and lung parenchyma with the formation of emphysema;
progressive bronchial obstruction.
If the first two positions can be established during the initial examination of the patient, then the progression can be most clearly confirmed with long-term (within a year) observation of the patient.
11. Final diagnosis
On the basis of additional laboratory and instrumental research methods, the preliminary diagnosis is confirmed.
The main diagnosis: COPD, emphysematous type, severe course (stage III), exacerbation of moderate severity.
Complications: Emphysema of the lungs. Pneumosclerosis.
Concomitant diseases: Hypertensive disease, stage 3 with arterial hypertension, grade 2, risk 4. Peptic ulcer of the stomach and duodenal ulcer, remission. Dorsopathy of the thoracic spine. Chronic hypertrophic laryngitis.
12. Etiology and pathogenesis
Risk factors:
1. Long-term exposure to airborne substances: (dust; chemical pollutants - vapors of acids, alkalis; industrial pollutants - SO2, NO2, black smoke.)
2. Environmental factors - air pollution in the atmosphere and premises (black smoke - SO2, smoke from cooking and fossil fuels, etc.). Contact with occupational hazards - cadmium, silicon, which are especially harmful. Increased harm in persons of the following professions: miners, construction workers in contact with cement, workers in contact with hot metal working, cotton growers, railway workers, etc. There is almost always an integration of external factors with internal ones - a genetic predisposition.
3. Hereditary predisposition (deficiency of neutrophil elastase inhibitors - alpha-1-antitrypsin, alpha-1-antichymotrypsin, alpha-2-macroglobulin.). The contribution of this cause to the occurrence of COPD is much less than that of smoking. Deficiency of alpha-1-antitrypsin leads to emphysema, COPD, and bronchiectasis.
4. Frequent inflammatory diseases of the respiratory system in early childhood, low birth weight. There are different points of view on the etiological significance of microorganisms in COPD, but the involvement of infection in the mechanism of development of COPD and the occurrence of exacerbations is undeniable. The main factors of bacterial colonization (settlement) are bacterial adhesion, weakening of mucociliary defense, damage to the integrity of the epithelium, and violation of local and systemic immunity. Infectious agents support inflammation in COPD not so much directly as through the activation of the main aggressor cells: neutrophils, macrophages, lymphocytes, etc.
Pathogenesis
The main consequence of the influence of etiological factors is the development of chronic inflammation. The localization of inflammation and the characteristics of the triggering factors determine the specificity of the pathological process in COPD. The effectiveness of mucociliary transport - the most important component of the normal functioning of the airways - depends on the coordination of the action of the ciliated apparatus of the ciliated epithelium, as well as the qualitative and quantitative characteristics of bronchial secretions. Under the influence of risk factors, the movement of cilia is disrupted until it stops completely, metaplasia of the epithelium develops with the loss of ciliary epithelial cells and an increase in the number of goblet cells. The composition of the bronchial secretion changes, which disrupts the movement of significantly thinned cilia. This contributes to the onset of mucostasis, which causes blockage of the small airways. Etiological factors of the external environment lead not only to disruption of mucociliary transport in the bronchi, but in parallel with this form oxidative stress, manifested by the formation of a large number of free radicals in the airways. The main source of free radicals are circulating blood neutrophils, which are concentrated in large numbers in the lungs under the influence of triggering factors. In conditions of high concentration of neutrophils, the balance of the protease - antiprotease system is disturbed. Along with neutrophils, macrophages and T-lymphocytes take part in the formation and implementation of inflammation. A biomarker of a chronic inflammatory process is the participation of neutrophils with increased activity of myeloperoxidase, neutrophil elastase, the appearance of metalloproteases, an imbalance in the proteolysis - antiproteolysis and oxidant - antioxidant systems. A large complex of pro-inflammatory mediators released from the cells infiltrating the mucous membrane accumulates in the pulmonary capillaries and peribronchial tissue and largely determines the entire variety of pathological changes. The main mediators of inflammation in COPD are interleukins, tumor necrosis factor, myeloperoxidases, neutrophil elastases, metalloproteases, and recently the role of defensins has been described. The change in the viscoelastic properties of the bronchial secretion is accompanied by significant qualitative changes in its composition: the content of nonspecific components of local immunity, which have antiviral and antimicrobial activity, decreases: interferon, lactoferin and lysozyme. Along with this, the content of secretory IgA decreases. Disorders of mucociliary clearance and the phenomenon of local immunodeficiency create optimal conditions for the colonization of microorganisms. Thick and viscous bronchial mucus with a reduced bactericidal potential is a good breeding ground for various microorganisms (viruses, bacteria, fungi). Under certain conditions, these patients are activated by a respiratory infection. This may be due to the reactivation of autoflora or superinfection with pneumotropic microorganisms, to which COPD patients are highly sensitive. This whole complex of mechanisms of inflammation leads to the formation of two main processes characteristic of COPD - impaired bronchial patency and the development of centrilobular emphysema. An essential link in the pathogenesis of impaired bronchial patency is the activation of cholinergic mechanisms of the autonomic nervous system, leading to an increase in bronchospastic reactions; the tone of the vagus nerve in patients with COPD increases in the early stages of the disease due to the excitation of irritative receptors of the bronchial epithelium. The irritating effect on the receptors is exerted by the effects of tobacco smoke, toxic gases (ozone, nitrogen dioxide, sulfur, etc.). The defeat of the epithelium is the initial link in inflammation.
Violation of bronchial patency in patients with COPD is formed due to reversible and irreversible components. The presence and severity of a reversible component gives individuality to the diseases that make up COPD, and allows them to be distinguished into separate nosological forms. The reversible component is formed from smooth muscle spasm, edema of the bronchial mucosa and mucus hypersecretion, arising under the influence of an increase in vagus nerve tone and the release of a large spectrum of pro-inflammatory mediators (interleukin-8, tumor necrosis factor, neutrophil proteases and free radicals). In the process of disease progression, the reversible component is gradually lost. With its complete loss, the disease changes its quality, and the boundaries of the nosological forms that make up COPD are erased. An irreversible component of bronchial obstruction is determined by developing emphysema and peribronchial fibrosis. Emphysema forms mainly as a result of depletion (due to oxidative stress) of local protease inhibitors and under the influence of neutrophilic proteases, which destroy the elastic stroma of the alveoli. Due to the violation of the elastic properties of the lungs, the mechanics of breathing change and expiratory collapse is formed, which is the most important cause of irreversible bronchial obstruction. Peribronchial fibrosis - a consequence of chronic inflammation, affects the formation of an irreversible component less than emphysema. The development of emphysema leads to a reduction in the vasculature in areas of the lung tissue that are not capable of gas exchange. As a result, the blood flow is redistributed in the remaining areas of the lung tissue, and pronounced ventilation-perfusion disorders occur. Unevenness of ventilation-perfusion relations is one of the important elements of the pathogenesis of COPD. Perfusion of poorly ventilated areas leads to a decrease in arterial oxygenation, excessive ventilation of insufficiently perfused areas leads to an increase in ventilation of the dead space and a delay in CO2 release. All this creates conditions for increasing pressure in the pulmonary artery basin. At this stage, pulmonary hypertension forms with the further development of cor pulmonale. Chronic hypoxia leads to compensatory erythrocytosis - secondary polycythemia with a corresponding increase in blood viscosity and microcirculation disorders, which aggravate ventilation-perfusion imbalances.
Aggravates bronchial obstruction and leads to an increase in all signs of the disease, exacerbation of the infectious process in the respiratory system. In conditions of mucostasis, local and sometimes systemic immunodeficiency, the colonization of microorganisms can take on an uncontrolled nature and move into a qualitatively different form of relationship with a macroorganism - an infectious process. Another way is also possible - the usual infection by airborne droplets with highly virulent flora, which is easily realized in conditions of disturbed protective mechanisms.
13. Clinical features of the course of the disease
Clinical features: gender (male), age (60 years), smoking.
14. Treatment
To stop the developed exacerbation, bronchodilators (B2-agonists, anticholinergics, methylxanthines), glucocorticoids, antibiotics, controlled oxygen therapy, non-invasive ventilation of the lungs, etc. are used.
Bronchodilators.
One of the main principles of treatment of exacerbation of COPD is intensification of bronchodilator therapy. Strengthening bronchodilator therapy is achieved by increasing doses and modifying drug delivery methods. Currently, the effectiveness of short-acting β2-agonists (salbutamol, fenoterol) and IB in patients with exacerbations of COPD has been proven. The preferred bronchodilators for acute exacerbations of COPD are short-acting β2-agonists.
As a bronchodilator therapy for an exacerbation of severe COPD, it is recommended to prescribe nebulized solutions of short-acting β2-agonists, for example, Ventolin 2.5-5 mg per inhalation. When treating severely ill patients with multiple organ pathology, tachycardia, hypoxemia, the role of ACP drugs increases. IB is prescribed both as monotherapy and in combination with β2-agonists (berodual solution).
Glucocorticosteroid drugs
It is generally accepted that with exacerbation of COPD, accompanied by a decrease in FEV1 of less than 50% of the proper values, glucocorticosteroids are prescribed in parallel with bronchodilator therapy. Therapy with systemic glucocorticosteroids (oral or parenteral) promotes a faster increase in FEV1, a decrease in shortness of breath, an improvement in arterial blood oxygenation, and a shorter hospital stay , as well as a decrease in the number of complications such as death from any cause, the need for intubation, repeated intensive therapy, etc. The GCS should be prescribed as early as possible, even upon admission to the emergency department. Oral or intravenous administration of glucocorticoids for exacerbations of COPD at the hospital stage is carried out in parallel with bronchodilator therapy (if indicated, in combination with antibiotics and oxygen therapy). Given the serious risk of developing adverse events with high-dose steroid therapy, 30-40 mg of prednisolone should be prescribed for 10-14 days . Further continuation of treatment does not lead to an increase in efficiency and at the same time increases the risk of developing adverse events.
Antibacterial agents
Indications for antibiotic therapy in patients with exacerbation of COPD are increased shortness of breath, increased sputum volume and purulent character . Taking into account the heterogeneity of patients undergoing exacerbation of COPD, it is advisable to distinguish separate groups of patients, for each of which we can most predict the list of probable pathogens and the prevalence of antibiotic-resistant strains.
Antibiotic therapy for exacerbation of COPD
|
Definition |
Main pathogens |
Antibacterial therapy |
||
|
Drugs of choice |
Alternative drugs |
|||
|
Simple (uncomplicated) exacerbation of COPD |
||||
|
Increased shortness of breath, increased volume and purulent sputum |
H.influenzae H.parainfluenzae S.pneumoniae M.catarrhalis Possible resistance to β-lactams |
Amoxicillin |
respiratory fluoroquinolones (levofloxacin) or "new" macrolides (azithromycin, clarithromycin), cefuroxime axetil (zinnat). |
|
|
Complicated exacerbation of COPD |
||||
|
Increased shortness of breath, increased volume and purulence of sputum. Frequent exacerbations\u003e 4 / yr Age\u003e 65 years |
H.influenzae H.parainfluenzae S.pneumoniae M.catarrhalis Probable resistance to β-lactams |
Amoxicillin + clavulanate (augmentin, amoxiclav), respiratory fluoroquinolones (levofloxacin) or cephalospirins of 2-3 generations (cefuroxime axetil or zinnat, claforan, etc.) |
The first group (uncomplicated exacerbation of COPD) includes patients under the age of 65 with infrequent exacerbations of the disease (less than 4 in a calendar year), the absence of serious concomitant diseases and minor or moderate impairments of bronchial patency (FEV1\u003e 50%). For this category of patients, the likely causative agents of exacerbation are H. influenzae, H. parainfluenzae, S. pneumoniae and M. catarrhalis with a natural level of sensitivity to antibiotics.
...Similar documents
The main complaints of the patient upon admission. History of the development of chronic obstructive pulmonary disease (COPD). Anamnesis of the patient's life, his present condition. Rationale for the diagnosis: emphysematous type of COPD, exacerbation stage. Prescribing treatment to the patient.
case history, added 12/19/2014
The concept and general characteristics of heart failure, the main causes and prerequisites for the development of this disease. Clinical picture and symptoms, etiology and pathogenesis, principles of diagnosis. Approaches to treatment regimen, prevention.
case history, added 12/23/2014
The concept and main causes of chronic obstructive pulmonary disease, its clinical signs and stages of development, symptoms. Methods for diagnosing this disease, principles and drawing up a scheme for its treatment, prevention and prognosis.
case history, added 11/26/2013
General characteristics and causes of the development of gallstone disease, its clinical picture and symptoms, etiology and pathogenesis. An examination plan for making a differential diagnosis, carrying out the necessary procedures and tests. Drawing up a treatment regimen.
case history, added 05/23/2014
Chronic obstructive bronchitis, pulmonary emphysema, severe forms of bronchial asthma. Major risk factors. Classification of chronic obstructive pulmonary disease (COPD) by severity. The main clinical characteristics and phases of the course of the types of COPD.
presentation added on 10/04/2015
The National Heart, Lung, and Blood Institute of the United States of America Global Chronic Obstructive Pulmonary Disease (COPD) Global Initiative. Development and approval of a global COPD control strategy. The clinical picture of the disease, its phenotypes and risk factors.
presentation added 02/22/2015
Pulmonary function tests, differential diagnosis of chronic obstructive disease: signs, clinical picture, results. The pathogenesis of COPD, in contrast to bronchial asthma: the nature of external respiration and shortness of breath; development factors, preventive measures.
presentation added on 11/12/2013
General characteristics, main causes of the appearance and factors of development of breast cancer. The clinical picture and symptoms of this disease, the stages and time frames of its development. Principles of diagnosis, treatment regimen, life prognosis.
case history, added 06/03/2014
Definition and risk factors for chronic obstructive pulmonary disease (COPD). Pathogenesis and forms of COPD course, clinical characteristics, course phases, diagnosis and treatment. Antibacterial drugs for exacerbations and inhaled bronchodilators.
presentation added on 10/04/2015
Diagnosis of the disease: chronic obstructive pulmonary disease, emphysematous type, exacerbation of moderate severity. Examination of the patient: conducting clinical analyzes, drawing up a conclusion, identifying the diagnosis. Patient treatment and observation.
DEFINITION.
Chronic obstructive pulmonary disease (COPD) is a disease characterized by a partially irreversible, steadily progressive restriction of airflow caused by an abnormal inflammatory response of the lung tissue to damaging environmental factors such as smoking, inhalation of particles or gases. The term "COPD" refers to a combination of chronic bronchitis and pulmonary emphysema.
Important provisions on COPD are set out in an international document drawn up by experts from 48 countries - "Global Initiative for the Treatment of Chronic Obstructive Pulmonary Disease - GOLD, 2003". Key points about COPD should be noted.
COPD has ceased to be a collective concept (chronic obstructive bronchitis, severe forms of bronchial asthma, obliterating bronchitis, cystic fibrosis, etc.);
COPD does not only refer to patients with terminal respiratory failure;
The concept of "chronic obstructive bronchitis" is absorbed by the concept of "chronic obstructive pulmonary disease".
RELEVANCE.
COPD is currently the fourth leading cause of death in the world with projected increases in prevalence and mortality in the coming decades. According to the Global Burden of Disease Study, the prevalence of COPD in 1990 was 9.34 per 1000 men and 7.33 per 1000 women (GOLD, 2003). Data on the prevalence, morbidity and mortality from COPD significantly underestimate the overall cost of the disease. COPD is usually not recognized or diagnosed until it becomes clinically significant. The significant increase in the widespread damage from COPD over the past 20 years reflects an increase in tobacco smoking, as well as a change in the age structure of the population.
Hoble risk factors. Internal factors:
Genetic factors (alpha-1-antitrypsin deficiency);
Airway hypersensitivity;
Lung growth.
External factors:
Smoking tobacco;
Professional dust and chemicals;
Domestic and outdoor air pollutants;
Infections;
Socio-economic status.
ETIOLOGY AND PATHOGENESIS.
The development of COPD can be hereditarily determined with congenital alpha-1-antitrypsin deficiency, but more often it is caused by active or passive smoking, air pollution, prolonged exposure to occupational factors (dust, vapors, chemical irritants), unfavorable home atmosphere (kitchen fumes, household chemicals ). The pathogenetic basis of COPD is a chronic inflammatory process of the tracheobronchial tree, pulmonary parenchyma and blood vessels, in which increased numbers of macrophages, T-lymphocytes and neutrophils are detected. Inflammatory cells secrete a large number of mediators: leukotriene B4, interleukin 8, tumor necrosis factor, and others that can damage the lung structure and maintain neutrophilic inflammation. In addition, an imbalance of proteolytic enzymes, antiproteinases, and oxidative stress are important in the pathogenesis of COPD.
Morphologically in the tracheobronchial tree, inflammatory cells infiltrate the superficial epithelium. The mucous glands expand and the number of goblet cells increases, leading to hypersecretion of mucus. In small bronchi and bronchioles, the inflammatory process occurs cyclically with structural remodeling of the bronchial wall, characterized by an increase in collagen and the formation of scar tissue, leading to persistent obstruction of the airways.
In the development of COPD, there is a sequential staging: the disease begins with mucus hypersecretion followed by impaired function of the ciliated epithelium, bronchial obstruction develops, which leads to the formation of emphysema, impaired gas exchange, respiratory failure, pulmonary hypertension and the development of cor pulmonale. The given data for reasons, pathogenesis, morphology show that COPD is the result of chronic bronchitis, prolonged bronchospastic syndrome and / or pulmonary emphysema and other parenchymal destruction (including congenital) associated with a decrease in the elastic properties of the lungs.
Chronic hypoxia leads to compensatory erythrocytosis - secondary polycythemia with a corresponding increase in blood viscosity and microcirculation disorders, which aggravate ventilation-perfusion imbalances.
An aggravation of the infectious process in the respiratory system leads to an increase in all signs of the disease. Under conditions of mucostasis, local and sometimes systemic immunodeficiency, the colonization of microorganisms can take on an uncontrolled nature and move into a qualitatively different form of relationship with a macroorganism - an infectious process. Another way is also possible - the usual infection by airborne droplets with highly virulent flora, which is easily realized in conditions of disturbed protective mechanisms. It should be emphasized that bronchopulmonary infection, although frequent, is not the only reason for the development of an exacerbation. Along with this, exacerbations of the disease are possible, associated with an increased effect of exogenous damaging factors, or in connection with inadequate physical activity. In these cases, signs of an infectious lesion of the respiratory system are minimal. As COPD progresses, the intervals between exacerbations become shorter.
COPD CLASSIFICATION(GOLD, 2003)
0 - the risk of developing the disease:
Normal spirometry;
Chronic symptoms (cough, sputum production);
I - mild course:
FEV 1 / FVC<70% от должного;
The presence or absence of chronic symptoms (cough, phlegm);
II - moderate course:
FEV 1 / FVC<70% от должного;
50% ≤ OFV 1<80% от должных значений;
III - severe course:
FEV 1 / FVC<70% от должного;
30% ≤ OFV 1<50% от должных значений;
The presence or absence of chronic symptoms;
IV - extremely severe course:
FEV 1 / FVC<70% от должного;
FEV 1 ≤30% of due or FEV 1<50% от должного в сочетании с хронической дыхательной недостаточностью (PaO2≤60% мм рт. ст. и/или PaCO 2 ≥ 50 мм рт. ст.);
The presence of cough, sputum, shortness of breath, clinical signs of right ventricular failure.
CLINIC.
The clinical picture of COPD is characterized by the same type of clinical manifestations - cough and shortness of breath, despite the heterogeneity of the diseases that make up it. The degree of their severity depends on the stage of the disease, the rate of progression of the disease and the predominant level of damage to the bronchial tree.
The rate of progression and severity of COPD symptoms depends on the intensity of exposure to etiological factors and their summation. Thus, the standards of the American Thoracic Society emphasize that the appearance of the first clinical symptoms in patients with COPD is usually preceded by smoking at least 20 cigarettes a day for 20 or more years.
The first signs with which patients usually go to the doctor are coughing and shortness of breath, sometimes accompanied by wheezing with sputum production. These symptoms are more pronounced in the morning.
The earliest symptom that appears by the age of 40-50 is cough. By the same time, in cold seasons, episodes of respiratory infection begin to appear, which are not initially associated with one disease. Dyspnea felt during exercise occurs on average 10 years after the onset of cough. However, in some cases, the onset of the disease from shortness of breath is possible.
Sputum is secreted in a small amount (rarely\u003e 60 ml / day) in the morning and has a slimy character. Exacerbations of an infectious nature are manifested by the aggravation of all signs of the disease, the appearance of purulent sputum and an increase in its amount.
Shortness of breath can vary very widely: from feeling short of breath during standard physical activity to severe respiratory failure.
Obstructive sleep apnea syndrome is observed in a number of patients with COPD. The combination of bronchial obstruction, characteristic of COPD, with sleep apnea is called overlap syndrom, in which gas exchange disturbances are most pronounced. It is believed that in the majority of patients, chronic hypercapnia is formed mainly at night.
There are two clinical forms of the disease - emphysematous and bronchitis.
The emphysematous form (type) of COPD is associated mainly with panacinar emphysema. Such patients are figuratively called "pink puffers", because to overcome the premature expiratory collapse of the bronchi, exhalation is performed through the lips folded into a tube and is accompanied by a kind of puffing. In the clinical picture, dyspnea prevails at rest due to a decrease in the diffusion surface of the lungs. Such patients are usually thin, their cough is often dry or with a small amount of thick and viscous sputum. The complexion is pink because adequate blood oxygenation is maintained by increasing ventilation as much as possible. The ventilation limit is reached at rest, and patients do not tolerate physical activity very well. Pulmonary hypertension is moderate, because reduction of the arterial bed caused by atrophy of interalveolar septa does not reach significant values. Cor pulmonale is compensated for a long time. Thus, the emphysematous type of COPD is characterized by the predominant development of respiratory failure.
The bronchitic form (type) is observed with centriacinar emphysema. Constant hypersecretion causes an increase in resistance during inspiration and expiration, which contributes to a significant violation of ventilation. In turn, a sharp decrease in ventilation leads to a significant decrease in the content of O 2 in the alveoli, a subsequent violation of the perfusion-diffusion ratios and blood shunting. This is what determines the characteristic blue tint of diffuse cyanosis in patients of this category. Such patients are obese, the clinical picture is dominated by cough with profuse sputum production. Diffuse pneumosclerosis and obliteration of the lumen of blood vessels lead to the rapid development of cor pulmonale and its decompensation. This is facilitated by persistent pulmonary hypertension, significant hypoxemia, erythrocytosis and constant intoxication due to a pronounced inflammatory process in the bronchi.
Isolation of two forms has prognostic value. So, in the emphysematous type in the later stages, there is a decompensation of cor pulmonale in comparison with the bronchitic variant of COPD. In clinical settings, patients with a mixed type of disease are more common.
COPD classification by severity identifies a number of stages in the course of the disease. Stage 0 means an increased risk of developing COPD. It is characterized by the onset of symptoms (cough, sputum production) with normal ventilation function of the lungs and actually corresponds to chronic bronchitis. With mild COPD ( stage I) and minimal clinical signs (cough, sputum) obstructive disorders are recorded. With moderate COPD ( stage II), more pronounced obstructive disorders of pulmonary ventilation are recorded, and in addition to cough and sputum, shortness of breath appears, which indicates the development of respiratory failure. In severe and extremely severe COPD ( stage III – IV) chronic respiratory failure and signs of cor pulmonale (right ventricular failure) are noted. Obstructive disorders detected in the study of the ventilation function of the lungs can reach critical values.
MAIN SIGNS TO SUSPECT COPD.
Chronic cough
Intermittent or daily. It often happens all day long.
Chronic sputum discharge
Any case of chronic sputum discharge may indicate COPD.
Dyspnea
Progressive, persistent. Aggravated by exercise and respiratory infections.
History of exposure to risk factors
Tobacco smoking, professional pollutants and chemicals. Smoke from the kitchen and home heating.
If any of these signs are present, COPD should be suspected and a respiratory function test should be performed.
Smoking history
A prerequisite for the diagnosis of COPD, according to the WHO recommendation, is the calculation of the smoking index. The calculation of the smoking index is carried out as follows: the number of cigarettes smoked per day is multiplied by the number of months in a year, i.e. by 12; if this value exceeds 160, then smoking in this patient poses a risk in relation to the development of COPD; if the values \u200b\u200bof this index are exceeded, more than 200 patients should be classified as "hard smokers".
It is recommended to calculate the smoking history in units of "packs / years". The smoking history should include the number of cigarettes smoked per day multiplied by the number of years and thus the total number of packs / years of smoking is calculated. At the same time, one pack contains 20 cigarettes and the number of cigarettes smoked per day for one year is equal to one pack / year.
Total packs / years \u003d number of cigarettes smoked per day x number of years / 20
It is believed that if this value exceeds 25 packs / years, then the patient can be classified as a "heavy smoker". In the event that this figure reaches 10 packs / years, then the patient is considered an "unconditional smoker". A patient is considered a "former smoker" in case of smoking cessation for a period of 6 months or more. This must be considered when diagnosing COPD.
Objective research.
The results of an objective study of patients with COPD depend on the severity of bronchial obstruction and emphysema.
Inspection. In the late stages of COPD, there are clinical signs of pulmonary emphysema (increased anteroposterior chest size, dilated intercostal spaces). With severe emphysema, the patient's appearance changes, a barrel-shaped chest appears. Due to the expansion of the chest and upward displacement of the collarbones, the neck seems short and thickened, the supraclavicular fossae are protruded (filled with expanded tops of the lungs). With the development of chronic respiratory failure and pulmonary hypertension, "warm" acrocyanosis, swollen neck veins are noted.
Percussion. In the presence of emphysema - percussion box sound, expansion of the boundaries of the lungs. In cases of severe emphysema, the absolute dullness of the heart may not be completely determined. The edges of the lungs are displaced downward, their mobility during breathing is limited. As a result, from under the edge of the costal arch, a soft, painless edge of the liver can protrude at its normal size.
Auscultation.In the lungs, scattered dry rales of various timbre are heard. As the disease progresses, wheezing is added to the cough, which is most noticeable with a rapid expiration. Sometimes auscultatory phenomena in the lungs are not detected and to identify them it is necessary to offer the patient to make a forced exhalation. The mobility of the diaphragm is limited with severe emphysema, which leads to a change in the auscultatory picture: weakened breathing appears, the severity of wheezing decreases, exhalation is lengthened.
The sensitivity of objective methods for determining the severity of COPD is low. Among the classic signs are wheezing exhalation and prolonged expiratory time (more than 5 s), which indicate bronchial obstruction.
DIAGNOSTICS.
Diagnostic methods can be conditionally divided into a mandatory minimum used in all patients, and additional methods used for special indications.
The mandatory methods, in addition to physical, include the determination of the function of external respiration (FVD), blood test, cytological examination of sputum, X-ray examination, blood test and ECG.
Laboratory research methods.
Sputum examination.
Cytological examination of sputum provides information on the nature of the inflammatory process and its severity. Required.
Microbiological (culture) examination of sputum is advisable to carry out with uncontrolled progression of the infectious process and the selection of rational antibiotic therapy. It is an additional examination method.
Blood test.
Clinical analysis. With a stable course of COPD, significant changes in the content of peripheral blood leukocytes do not occur. With exacerbation, neutrophilic leukocytosis with a stab shift and an increase in ESR are most often observed. However, these changes are not always observed.
With the development of hypoxemia in patients with COPD, polycythemic syndrome is formed, which is characterized by a change in hematocrit (hematocrit\u003e 47% in women and\u003e 52% in men), an increase in the number of red blood cells, a high level of hemoglobin, low ESR and increased blood viscosity.
X-ray examination organs of the chest is a mandatory examination method. Radiography of the lungs in frontal and lateral projections in COPD reveals an increase in the transparency of the lung tissue, a low standing of the dome of the diaphragm, a limitation of its mobility, an increase in the retrosternal space, which is characteristic of emphysema.
With mild COPD, significant radiographic changes may not be detected. In patients with moderate and severe COPD, it is possible to detect a low standing of the dome of the diaphragm, flattening and limiting its mobility, hyper-airiness of pulmonary fields, bullae and an increase in the retrosternal space; narrowing and elongation of the heart shadow; against the background of depletion of vascular shadows, a high density of the walls of the bronchi is determined, infiltration along their course, i.e. a number of signs are revealed that characterize the inflammatory process in the bronchial tree and the presence of emphysema.
CT scan lungs is an additional method and is carried out according to special indications. It allows you to quantitatively determine the morphological changes in the lungs, first of all, emphysema, to more clearly identify the bullae, their localization and size.
Electrocardiography allows to identify signs of hypertrophy of the right heart in a number of patients, however, its ECG criteria change sharply due to emphysema. ECG data in most cases allow to exclude the cardiac genesis of respiratory symptoms.
Bronchological examination (fibrobronchoscopy) is optional for patients with COPD. It is carried out to assess the condition of the bronchial mucosa and differential diagnosis with other lung diseases. In some cases, diseases that are the cause of chronic bronchial obstruction can be identified.
Research should include:
Examination of the bronchial mucosa;
Cultural examination of bronchial contents;
Bronchoalveolar lavage with determination of cellular composition to clarify the nature of inflammation;
Biopsy of the bronchial mucosa.
Examination of the function of external respiration (spirography) is of leading importance in the diagnosis of COPD and an objective assessment of the severity of the disease. It is obligatory to determine the following volumetric and velocity indicators: vital capacity of the lungs (VC), forced vital capacity of the lungs (FVC), forced expiratory volume in 1 second (FEV 1), maximum expiratory flow rate at 75, 50 and 25% (MSV 75- 25). The study of these indicators forms functional diagnosis of COPD.
Functional disorders in COPD are manifested not only by impaired bronchial patency, but also by changes in the structure of static volumes, impaired elastic properties, diffusion capacity of the lungs, and decreased physical performance. The definition of these groups of disorders is optional.
Violation of bronchial patency.The most important thing for the diagnosis of COPD is the determination of chronic airflow restriction, i.e. bronchial obstruction. The main criterion for determining chronic airflow restriction, or chronic obstruction, is the fall in FEV 1 to a level that is less than 80% of the required values. Bronchial obstruction is considered chronic if it is recorded during repeated spirometry studies at least 3 times within one year, despite ongoing therapy.
To study the reversibility of obstruction, samples with inhaled bronchodilators are used, and their effect on the flow-volume curve, mainly on the forced expiratory volume in 1 second (FEV 1) is assessed. When examining a particular patient with COPD, it should be remembered that the reversibility of obstruction is a variable value. and in the same patient it can be different during periods of exacerbation and remission.
Bronchodilator tests... As bronchodilatory drugs when conducting tests in adults, it is recommended to prescribe:
Beta 2 - short-acting agonists (starting from the minimum dose to the maximum allowable: fenoterol - from 100 to 800 mcg; salbutamol - from 200 to 800 mcg, terbutaline - from 250 to 1000 mcg) with measurement of the bronchodilatory response after 15 minutes;
Anticholinergic drugs - it is recommended to use ipratropium bromide as a standard drug, starting from the minimum dose of 40 μg to the maximum possible dose of 80 μg, with the measurement of the bronchodilatory response after 30-45 minutes.
It is possible to conduct bronchodilatory tests by prescribing higher doses of drugs that are inhaled through nebulizers.
In order to avoid distortion of the results and for the correct performance of the bronchodilation test, it is necessary to cancel the ongoing therapy in accordance with the pharmacokinetic properties of the drug taken (beta-2 - short-acting agonists - 6 hours before the start of the test, long-acting beta-2 - agonists - in 12 hours, prolonged theophyllines - in 24 hours).
An increase in FEV 1 by more than 15% of the baseline values \u200b\u200bis conventionally characterized as reversible obstruction.
FEV monitoring 1 . An important method for confirming the diagnosis of COPD is monitoring FEV 1 - a long-term repeated measurement of this spirometric indicator. In adulthood, an annual fall in FEV 1 within 30 ml per year is normally noted. Large epidemiological studies carried out in different countries made it possible to establish that patients with COPD are characterized by an annual drop in the FEV 1 index of more than 50 ml per year.
Blood gas composition. COPD is accompanied by a violation of ventilation-perfusion ratios, which can lead to arterial hypoxemia - a decrease in oxygen tension in arterial blood (PaO2). In addition, ventilation respiratory failure leads to an increase in the carbon dioxide voltage in arterial blood (PaCO2). In patients with COPD with chronic respiratory failure, the onset of acidosis is metabolically compensated by increased production of bicarbonate, which allows maintaining a relatively normal pH level.
Pulse Oximetry It is used to measure and monitor blood oxygen saturation (SaO2), but it only allows recording the level of oxygenation and does not allow monitoring changes in PaCO2. If the SaO2 is less than 94%, then a blood gas test is indicated.
With the progression of COPD, an increase in pressure in the pulmonary artery is often observed.
The severity of pulmonary hypertension has prognostic value. Among non-invasive methods for controlling pulmonary hypertension, the best results were obtained using doppler echocardiography... In routine management of COPD patients, the use of direct pulmonary artery pressure measurements is not recommended.
Differential diagnosis.
At the early stages of the development of COPD, one should distinguish between chronic obstructive bronchitis (COP) and bronchial asthma (BA), since at this time fundamentally different approaches to the treatment of each of these diseases are required.
Clinical examination reveals paroxysmal symptoms in AD, often with a combination of extrapulmonary signs of allergy (rhinitis, conjunctivitis, skin manifestations, food allergy). Patients with COB are characterized by constant, little-changing symptoms.
An important element of differential diagnosis is a decrease in FEV 1 by 50 ml in patients with COB, which is not observed in BA. COB is characterized by decreased daily variability of peak flow metrics.< 15%. При БА разность между утренними и вечерними показателями пикфлоуметрии повышена и превышает 20%. При БА чаще наблюдается бронхиальная гиперреактивность. Из лабораторных признаков при БА чаще встречается увеличение содержания IgЕ. При появлении у больных БА необратимого компонента бронхиальной обструкции, дифференциальный диагноз этих заболеваний теряет смысл, так как можно констатировать присоединение второй болезни – ХОБ и приближение конечной фазы заболевания – ХОБЛ.
TREATMENT.
The goal of treatment is to reduce the rate of progression of the disease leading to an increase in bronchial obstruction and respiratory failure, to reduce the frequency and duration of exacerbations, to increase exercise tolerance and improve the quality of life.
Patient education - a crucial stage of individual work with a patient. The patient should be well aware of the nature of the disease, the characteristics of its course, be an active, conscious participant in the treatment process. Educational programs for patients necessarily include training in the correct use of drugs (individual inhalers, spacers, nebulizers). Patients should be trained in the basic rules of self-control, including the use of a peak flow meter, should be able to objectively assess their condition and, if necessary, take emergency self-help measures. An important stage in the education of patients is their professional orientation, especially in cases where environmental aggression is associated with the patient's professional activity.
Smoking cessation Is the first required step. The patient should be clearly aware of the harmful effects of tobacco smoke on his respiratory system. A specific smoking restriction and cessation program is being drawn up. In cases of nicotine addiction, it is advisable to use nicotine-substituting drugs. It is possible to attract psychotherapists, acupuncturists. The positive effect of quitting smoking is expressed at any stage of COPD.
Bronchodilatory therapy.
According to modern concepts of the essence of COPD, bronchial obstruction is the main and universal source of all pathological events that develop with the constant progression of the disease and lead to respiratory failure.
The use of bronchodilator drugs is the basic therapy that is mandatory in the treatment of patients with COPD. All other means and methods should be used only in combination with basic therapy means.
Preference is given to the use of inhaled forms of bronchodilators. The inhalation route of administration of drugs contributes to a more rapid penetration of the drug into the affected organ, therefore, a more effective drug action. At the same time, the potential risk of developing side systemic effects is significantly reduced. The use of a spacer allows: to facilitate the implementation of inhalation, to increase its effectiveness, to further reduce the potential risk of developing systemic and local side effects.
The optimal today is the use of powder inhalers or bronchodilators in solutions for nebulizer therapy.
Of the existing bronchodilators, m-anticholinergics, beta-2-agonists, and methylxanthines are used in the treatment of COPD; the sequence of use and the combination of these funds depends on the severity of the disease, the individual characteristics of its progression.
Traditionally, basic bronchodilators for the treatment of COPD are considered m-anticholinergics... They are represented by ipratropium bromide (duration of action 6-8 hours) and a combined bronchodilator - berodual (ipratropium bromide + fenoterol). Currently, a new anticholinergic with prolonged action, tiotropium bromide (spiriva), has appeared, which is applied once a day.
Are used selective sympathomimetics (beta-2 agonists) short (4-6 hours) action: fenoterol, salbutamol, terbutaline. The action of sympathomimetics occurs quickly, but they are characterized by a number of systemic side effects due to the effect on the cardiovascular system. With age, the sensitivity of receptors to sympathomimetics decreases. In recent years, for the relief of bronchial obstruction and basic therapy of COPD, a new drug from the group of beta-2-agonists, oxis turbuhaler, has become widely used - the active ingredient of which is formoterol, which has not only a quick onset of action (after 1-3 minutes), but also a long one. effect (for 12 hours or more).
Theophylline prolonged action (teotard, teopec) are effective in the treatment of COPD and are currently used quite widely both as monotherapy and in addition to sympathomimetics. But due to their narrow borderline between therapeutic and toxic doses, preference is given to inhaled bronchodilators.
In stage I COPD, short-acting bronchodilators are used on demand. In stages II – IV, the systematic use of one bronchodilator (or a combination of drugs), short or long acting, with a rapidly occurring effect is prescribed. Inhaled corticosteroids are used if their clinical and ventilation performance is significantly improved.
Mucoregulatory agents... An improvement in mucociliary clearance is largely achieved with a targeted effect on bronchial secretions using mucoregulatory drugs.
The use of proteolytic enzymes as mucolytic agents is unacceptable due to the high risk of developing serious side effects - hemoptysis, allergies, bronchoconstriction. Ambroxol (ambrosan, lazolvan) stimulates the formation of tracheobronchial secretions of reduced viscosity due to depolymerization of acidic mucopolysaccharides of bronchial mucus and the production of neutral mucopolysaccharides by goblet cells.
A distinctive feature of the drug is its ability to increase the synthesis, secretion of surfactant and block the breakdown of the latter under the influence of unfavorable factors.
When combined with antibiotics, Ambroxol enhances their penetration into the bronchial secretions and the bronchial mucosa, increasing the effectiveness of antibiotic therapy and reducing its duration. The drug is used internally and by inhalation.
Acetylcysteine free from the damaging action of proteolytic enzymes. The sulfhydryl groups of its molecules break the disulfide bonds of mucopolysaccharides in sputum. Stimulation of mucosal cells also leads to dilution of sputum. Acetylcysteine \u200b\u200bwill increase the synthesis of glutathione, which is involved in detoxification processes. It is used inside and in inhalation.
Carbocisteine normalizes the quantitative ratio of acidic and neutral sialomucins of bronchial secretions. Under the influence of the drug, regeneration of the mucous membrane occurs, a decrease in the number of goblet cells, especially in the terminal bronchi, i.e. the drug has muco-regulating and mucolytic effects. This restores the secretion of IgA and the number of sulfhydryl groups. It is used internally.
Glucocorticosteroid therapy. The indication for the use of GCS in COPD is the ineffectiveness of the maximum doses of the basic therapy - bronchodilators. GCS, so effective in the treatment of bronchial asthma, are used in the treatment of COPD only with a proven clinical or spirometric effect. A reversibility test has been formulated to predict the advisability of prescribing corticosteroids: after the initial determination of FEV 1, corticosteroids are administered orally (for 1–2 weeks) or inhalation (for a period of 6–12 weeks). An increase in FEV 1 by 15% (or 200 ml) after trial use of steroids is considered a positive result and gives rise to long-term therapy with inhaled corticosteroids. This test can also be performed using peak flowmetry (an increase in expiratory power by 20% is considered positive).
The use of GCS in tablets for more than 2 weeks is undesirable. It is optimal to use inhaled GCS or solutions (suspensions) for nebulizers (for example, Pulmicort suspension). In severe and extremely severe COPD ( stage III – IV) as a basic therapy, it is recommended to use the combined drug symbicort, which includes corticosteroids budesonide and a long-acting beta-2-agonist formoterol.
In the treatment of moderate to severe exacerbations of COPD, nebulizer therapy is necessary. The nebulizer enables the inhalation of bronchodilators and glucocorticosteroid hormones in high doses.
Respiratory failure correction achieved through the use of oxygen therapy, training of the respiratory muscles. It should be emphasized that the intensity, volume and nature of drug treatment depend on the severity of the condition and the ratio of reversible and irreversible components of bronchial obstruction. With the depletion of the reversible component, the nature of the therapy changes. In the first place are methods aimed at correcting respiratory failure. At the same time, the volume and intensity of the basic therapy are preserved.
Indication for systematic oxygen therapy is a decrease in the partial tension of oxygen in the blood - PaO2 to 60 mm Hg. Art., decrease in oxygen saturation - SaO2< 85% при стандартной пробе с 6-минутной ходьбой и < 88% в покое. Предпочтение отдается длительной (18 часов в сутки) малопоточной (2-5 л в мин) кислородотерапии как в стационарных условиях, так и на дому. При тяжелой дыхательной недостаточности применяются гелиево-кислородные смеси. Для домашней оксигенотерапии используются концентраторы кислорода, а также приборы для проведения неинвазивной вентиляции с отрицательным и положительным давлением на вдохе и выдохе.
Respiratory muscle training is achieved with the help of individually selected breathing exercises. It is possible to use percutaneous electrical stimulation of the diaphragm.
In severe polycythemic syndrome (Hb\u003e 155 g / l), erythrocytaphoresis with the removal of 500-600 ml of deplasmed erythrocyte mass. If erythrocytaphoresis is not technically feasible, bloodletting in a volume of 800 ml of blood with adequate replacement with isotonic sodium chloride solution or herudotherapy (treatment with leeches).
Antibacterial therapy. During the period of stable COPD, antibiotic therapy is not performed.
In the cold season, patients with COPD often experience exacerbations of an infectious origin. The most common causes are Streptococcus pneumonia, Haemophilus influenzae, Moraxella catarralis and viruses. Antibiotics are prescribed in the presence of clinical signs of intoxication, an increase in the amount of sputum and the appearance of purulent elements in it. Usually, treatment is prescribed empirically with drugs inside and lasts 7-14 days, with severe exacerbation, parenteral administration is used.
Taking into account the specified spectrum of microorganisms, apply:
aminopenicillins inside (amoxicillin),
cephalosporins II-III generations (cefuroxime orally, ceftriaxone - parenterally),
new macrolides inside (spiramycin, clarithromycin, azithromycin, midecamycin),
respiratory (pneumotropic) fluoroquinolones of III-IV generations (levofloxacin).
The selection of an antibiotic according to the sensitivity of the flora in vitro is carried out only if empirical antibiotic therapy is ineffective.
Inhaled antibiotics should not be prescribed.
Vaccinationagainst influenza (Vaxigrip, influenza, influenza, begrivac, etc.), against pneumococcus (pneumo 23) allows to reduce the number of exacerbations of the disease and the severity of their course, thereby reducing the number of days of disability and improving bronchial patency. It is recommended that annual prophylactic vaccination against influenza in patients with COPD with mild and moderate severity of the disease and the frequency of infectious relapses is more than 2 times a year. A single vaccination pneumo 23 is effective for 5 years, then revaccination is carried out every 5 years.
Rehabilitation therapy.
Rehabilitation therapy is prescribed for COPD of any severity. The doctor determines an individual rehabilitation program for each patient. Depending on the severity, phase of the disease and the degree of compensation of the respiratory and cardiovascular systems, the program includes a regimen, exercise therapy, physiotherapeutic procedures, and spa treatment.